Medication-Alcohol Interaction Checker
Check Your Alcohol-Medication Risk
One standard drink = 14g ethanol. All alcohol types carry the same risk with medications.
Select your medication and alcohol type to see risk assessment.
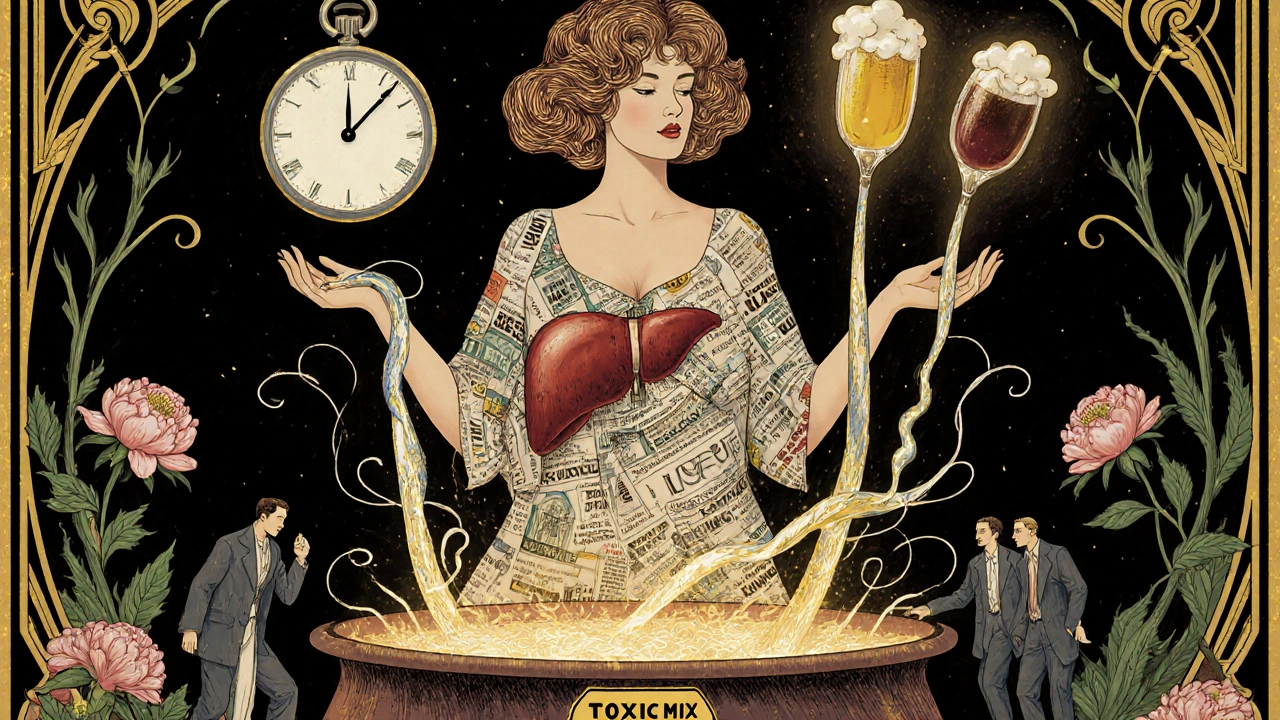
It’s not just about how much you drink-it’s about what you’re drinking with. Millions of people take medications every day and sip alcohol without realizing they’re putting their health at risk. Whether it’s a glass of wine with dinner, a beer after work, or a shot of whiskey before bed, the danger isn’t in the type of drink-it’s in the ethanol inside it. And yet, most people still think red wine is safer than spirits, or that beer won’t hurt because it’s "weaker." That’s a myth with deadly consequences.
One Drink, Same Risk-No Matter the Bottle
A 12-ounce beer, a 5-ounce glass of wine, and a 1.5-ounce shot of vodka all contain the same amount of pure alcohol: 14 grams. That’s one standard drink. And when it comes to how your body reacts with medication, that’s all that matters. Your liver doesn’t care if the alcohol came from a pint of lager, a bottle of Chardonnay, or a bottle of bourbon. It processes ethanol the same way every time-through enzymes called ADH and ALDH. These same enzymes break down dozens of common medications, from painkillers to antidepressants. When alcohol shows up, it fights for space. The result? Medications build up in your system, or get broken down too fast, turning safe doses into dangerous ones.
Studies from the National Institute on Alcohol Abuse and Alcoholism show that 40% of adults regularly mix alcohol with prescription drugs. And here’s the kicker: 67% of them have no idea it’s risky. That’s not ignorance-it’s misinformation. People hear "alcohol" and think of binge drinking. But even one drink can trigger a reaction.
Spirits: Fast, Strong, and Dangerous
Spirits get a bad reputation, and for good reason. A shot of whiskey hits your bloodstream faster than a beer because it’s consumed quickly and has no carbonation or volume to slow absorption. Emergency room data shows 68% of alcohol-medication overdose cases involve spirits. Why? Because people think, "It’s just one shot." But that one shot delivers the same ethanol as three beers-done in seconds. When you take a shot with a sleep aid like benzodiazepines, your brain gets hit with double the sedation. Research from the Illinois Poison Center found that a BAC of just 0.08% (easily reached with one shot) can make sedatives 300-500% stronger. That’s not a hangover. That’s respiratory depression. That’s a trip to the ER.
And it’s not just about quantity. Spirits often contain congeners-chemical byproducts from fermentation and aging. Darker spirits like bourbon and rum have more of these. While they don’t change how alcohol interacts with most meds, they can make nausea, vomiting, and dizziness worse. That’s why people on antibiotics like metronidazole report violent reactions after even a small amount of dark liquor. It’s not the alcohol alone-it’s the combo.
Wine: The "Healthier" Myth That Kills
Red wine gets marketed as heart-healthy. But when you’re on medication, that label doesn’t matter. Some people believe red wine is safer because of antioxidants like resveratrol. That’s not how it works. The polyphenols in red wine don’t protect you from alcohol’s effect on your liver or brain. In fact, one Mayo Clinic study found red wine increased bleeding risk with warfarin by 15% compared to the same amount of ethanol from spirits. Why? Because wine contains natural compounds that thin the blood. Add that to warfarin, and you’re playing Russian roulette with internal bleeding.
And then there’s the metronidazole factor. If you’re on this antibiotic for an infection, even a sip of wine can trigger a disulfiram-like reaction: flushing, pounding heart, vomiting, dizziness. It’s not an allergy. It’s a chemical explosion in your body. One study showed 82% of patients who drank wine while on metronidazole had severe symptoms. And yet, 41% of users still believe red wine is "safer" than other alcohol. That belief leads to more harm-not less.

Beer: The Silent Killer
Beer is the most dangerous alcohol type-not because it’s strong, but because it’s underestimated. People drink three, four, five beers thinking, "It’s just beer." But each one is a standard drink. Five beers? That’s five standard drinks. That’s enough to push your BAC into the danger zone with almost any medication. The CDC reports beer accounts for 52% of total ethanol consumed in the U.S. and 47% of unintentional alcohol-medication interactions. Why? Because it’s easy to drink slowly over hours. You don’t feel drunk. You feel fine. But your liver is still overwhelmed.
And when beer meets NSAIDs like ibuprofen or naproxen? That’s a recipe for stomach bleeding. Alcohol irritates the stomach lining. NSAIDs do too. Together, they’re a one-two punch. GoodRx user reviews show 63% of people who mixed beer with painkillers ended up with ulcers or internal bleeding. They didn’t binge. They just had "a few with dinner." That’s all it takes.
Acetaminophen and Alcohol: A Silent Liver Bomb
Even if you’re not on a prescription, mixing alcohol with common over-the-counter painkillers like Tylenol (acetaminophen) is a silent killer. Every time you drink, your liver uses up glutathione to detoxify alcohol. When you take acetaminophen, your liver needs glutathione again to break it down. If you’ve been drinking-even just two drinks-the supply runs out. That’s when toxic byproducts build up and start destroying liver cells. Two standard drinks can increase liver damage risk by 300%. It doesn’t matter if it’s beer, wine, or whiskey. The math is the same. And you won’t feel it until it’s too late.
What About Non-Alcoholic Beer?
"It’s non-alcoholic, so it’s safe," people say. Not quite. Non-alcoholic beer still contains up to 0.5% alcohol. That’s not enough to get you drunk. But it’s enough to interfere with certain medications-especially those with narrow therapeutic windows like lithium, some seizure meds, or antipsychotics. One study found 18% of adults didn’t realize even non-alcoholic beer could cause interactions. That’s a dangerous gap in knowledge. If your doctor says "avoid alcohol," they mean any drink with ethanol-even if it’s labeled "0.5%".
What Should You Do?
The safest answer? Don’t drink at all when you’re on medication. But if you do, here’s what you need to know:
- One drink = one drink. No matter the type.
- Check your medication label. If it says "avoid alcohol," it means ALL alcohol.
- Never mix alcohol with benzodiazepines, opioids, sleep aids, antidepressants, or blood thinners.
- Use a standard drink chart. Know what 12 oz beer, 5 oz wine, and 1.5 oz spirits look like.
- Ask your pharmacist. They’re trained to spot these risks. Don’t assume your doctor told you everything.
Pharmacists now spend an average of 7.2 minutes per patient explaining this. That’s how important it is. And new systems in hospitals are starting to flag alcohol-medication risks during prescription processing. But you can’t wait for technology to save you. You have to be the first line of defense.
Real Stories, Real Risks
Reddit threads are full of people who thought they were fine. One user took a shot of whiskey with Xanax because "I just needed to sleep." Woke up in the hospital with low oxygen. Another drank two beers with ibuprofen for back pain and ended up in surgery for a bleeding ulcer. A woman on warfarin had a glass of red wine with dinner and nearly died from internal bleeding. These aren’t outliers. They’re predictable outcomes of misinformation.
You don’t need to be a heavy drinker to be at risk. You just need to believe the myth that "it’s just one"-and that the type of alcohol changes the rules. It doesn’t.
What’s Changing in 2025?
The FDA is pushing for new labeling rules that require drug manufacturers to specify alcohol interaction risks by beverage type. Hospitals are rolling out real-time alerts in electronic health records that warn doctors if a patient is prescribed a high-risk med and has a history of drinking. Apps like GoodRx now let you scan your meds and input what you drank-and they’ll tell you if it’s dangerous.
But the biggest change? Awareness. The CDC’s 2023 National Action Plan has made alcohol-medication interactions a top-five priority. And they’re spending $15 million to fix the confusion around "what counts as alcohol." Because the problem isn’t the drink. It’s the belief that some drinks are safe.
They’re not.


Dana Dolan 18.11.2025
Just had a glass of wine with my blood pressure med and now I’m sweating bullets. Not kidding. My heart felt like it was trying to escape my chest. I thought red wine was ‘healthy’-turns out it’s just a sneaky little traitor.
Thanks for this post. I’m never doing that again.
river weiss 18.11.2025
It is imperative to underscore that ethanol, regardless of its source, is metabolized by the same hepatic enzymatic pathways-namely alcohol dehydrogenase and aldehyde dehydrogenase-and its presence competitively inhibits the metabolism of numerous pharmaceutical agents, thereby increasing serum concentrations and potential toxicity. This is not a matter of opinion; it is a biochemical reality.
Zac Gray 18.11.2025
Oh wow, so the only difference between a shot of bourbon and a pint of beer is how fast you pass out? I mean, I get it, the math is the same-but have you ever tried explaining that to your buddy who thinks "it’s just one beer" while chugging four in an hour? He’s not dumb-he just thinks he’s invincible. And honestly? So am I, until I remember I’m on Zoloft and my liver is a sobbing mess.
Also, non-alcoholic beer? Bro, I drank one of those after surgery and my pharmacist gave me a look like I’d just set fire to the pharmacy. Turns out, 0.5% is enough to make lithium go full nuclear. Who knew?
Steve and Charlie Maidment 18.11.2025
Why do we even need a post like this? People are just too lazy to read the tiny print on their pill bottles. I mean, come on. If your meds say "avoid alcohol," isn’t that enough? Why do we need a 2000-word essay on how beer is a silent killer? It’s like writing a whole book about why you shouldn’t stick your finger in a live socket. Some things just shouldn’t need explaining.
Also, I’m pretty sure the FDA doesn’t care what kind of alcohol you drink. They just want you to stop being an idiot.
Michael Petesch 18.11.2025
Fascinating. In Japan, the cultural understanding of alcohol and medication is markedly different. Many elderly patients are explicitly warned by physicians against even one glass of sake with their antihypertensives. The concept of "standard drink" is rarely used; instead, the focus is on total ethanol volume and timing relative to dosing. It’s interesting how Western discourse focuses on beverage type, while Eastern systems emphasize pharmacokinetic timing. Perhaps we could learn from this.
Chuck Coffer 18.11.2025
So you’re telling me the only reason people drink wine instead of whiskey is because they think it makes them look classy? Congrats. You’ve just described every person who’s ever died from a bleeding ulcer while sipping Pinot Noir at a dinner party. You’re not a connoisseur. You’re a walking overdose waiting to happen.
Marjorie Antoniou 18.11.2025
I’m a nurse, and I’ve seen too many people come in thinking they’re fine because they "only had one drink." One drink is all it takes. One drink with warfarin. One drink with tramadol. One drink with Zoloft. It’s not about being a heavy drinker. It’s about being unaware. Please, if you’re on meds-just say no. Your body will thank you. And if you’re reading this and you’re the one who’s been ignoring this warning? I’m not mad. I’m just sad for you.
Andrew Baggley 18.11.2025
Hey, I used to mix beer with ibuprofen like it was nothing. Then I ended up in the ER with a bleeding ulcer. Didn’t even feel it coming. Now I don’t drink at all when I’m on meds. It’s not about being perfect-it’s about being alive. You don’t need to be a saint. Just be smart. One drink isn’t worth a hospital stay. Seriously. Your future self will thank you.
Frank Dahlmeyer 18.11.2025
Let me tell you something-my granddad used to say, "If it’s in a bottle and it burns, don’t mix it with your pills." He never went to college, never read a study, but he knew more about safety than half the doctors I’ve met. That’s the thing: wisdom doesn’t need a citation. It just needs experience. And if you’re still drinking wine with your blood thinner, you’re not being cultured-you’re being reckless. And no, I don’t care if it’s organic or from a vineyard in Tuscany. It’s still ethanol. It’s still dangerous. And your liver doesn’t care about the label.
Codie Wagers 18.11.2025
It’s not about alcohol. It’s about control. The entire modern world is built on the illusion of safety: non-alcoholic beer, "light" meds, "safe" doses. But your body doesn’t negotiate. It doesn’t care if you’re "responsible." It doesn’t care if you "only had one." It reacts. It burns. It fails. And then you wake up in a hospital wondering why your liver gave up. The truth? You gave up first. You chose the myth over the mechanism. And now you’re surprised when the mechanism wins?
Paige Lund 18.11.2025
So basically, if I want to live, I can’t have a glass of wine with dinner, a beer after work, or a shot before bed? Cool. I’ll just stick to water and existential dread. Thanks for the life update.
Andy Feltus 18.11.2025
What if the real issue isn’t the alcohol? What if it’s the fact that we’ve outsourced our health to pills and then treat our bodies like machines that can be tinkered with? We take a pill to fix something, then we pour ethanol into the system like it’s fuel, and we’re shocked when the engine blows? Maybe we’re not just mixing drugs and alcohol-we’re mixing denial with convenience. And the alcohol? It’s just the mirror.
Dion Hetemi 18.11.2025
People who think red wine is "safer" are the same people who think "natural" means "not toxic." Resveratrol doesn’t cancel out ethanol. It’s like putting a Band-Aid on a bullet wound and calling it a health hack. You’re not healing. You’re deluding. And if you’re still drinking while on metronidazole? You’re not a rebel. You’re a liability. And your doctor is probably tired of cleaning up your mess.
Kara Binning 18.11.2025
As an American, I find it offensive that people think non-alcoholic beer is dangerous. We invented beer. We invented freedom. We invented the right to drink whatever we want, whenever we want, with whatever meds we’re on. If you’re too weak to handle one sip of "0.5%" while on lithium, maybe you shouldn’t be on lithium. Or maybe you should move to Canada. They’re all about safety there. Too bad we’re not.
Brian Rono 18.11.2025
Let me be the first to say it: this whole post is just fearmongering dressed up as science. You’re equating one drink with a death sentence. Where’s the data on the 99% of people who drink one beer with their meds and live to tell the tale? You’re painting everyone as a walking time bomb. That’s not education. That’s moral panic. And it’s lazy. If you want people to listen, stop screaming. Start explaining. And for God’s sake, stop pretending a shot of whiskey is somehow more evil than a six-pack. They’re both ethanol. The difference? One’s got a better marketing team.