Anticholinergic Burden Calculator
Medication Selection
Select medications you're currently taking. First-generation antihistamines have high anticholinergic burden.
Selected Medications
0 totalYour Anticholinergic Burden
Recommendations
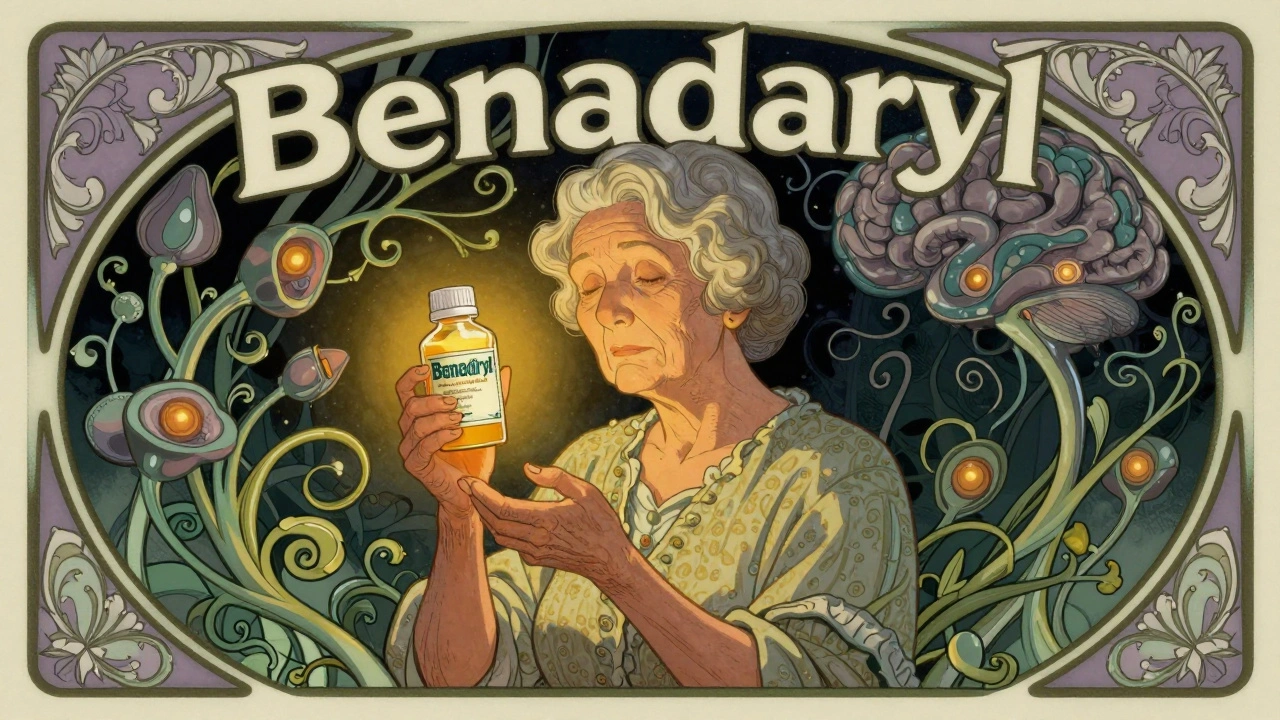
For years, millions of older adults have reached for over-the-counter antihistamines like Benadryl to help them sleep, relieve allergies, or calm an upset stomach. It’s cheap, easy to find, and seems harmless. But what if that nightly pill could be quietly affecting your brain? New research is raising serious questions about long-term use of certain antihistamines and their link to dementia risk - especially in people over 65.
Not All Antihistamines Are the Same
There are two main types of antihistamines: first-generation and second-generation. The difference isn’t just about brand names - it’s about what happens inside your body.First-generation antihistamines like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine cross the blood-brain barrier. Once there, they block acetylcholine, a key chemical your brain uses to form memories, focus attention, and regulate sleep cycles. This is called anticholinergic activity. It’s why these drugs make you drowsy - and why they can mess with your thinking over time.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed differently. They don’t easily enter the brain. Their anticholinergic effect is so weak - up to 1,000 times less than first-gen drugs - that they’re considered nearly neutral for cognitive risk. If you’re taking an antihistamine regularly, switching to one of these could be one of the simplest, safest changes you make.
The Evidence Is Mixed - But the Warnings Are Real
A 2015 study from JAMA Internal Medicine shook up the medical world. Researchers tracked over 3,400 people aged 65 and older for a decade. They found that those who took anticholinergic drugs - including first-gen antihistamines - for the equivalent of three or more years had a higher chance of developing dementia. The study didn’t say antihistamines caused dementia. But it did show a clear pattern: the longer you take them, the higher the risk.But here’s where it gets complicated. A 2019 follow-up study looked at different drug classes separately. It found that antidepressants, bladder meds, and Parkinson’s drugs had strong links to dementia risk. But antihistamines? No significant connection. Another 2022 study of nearly 9,000 seniors found dementia rates were slightly higher in those using diphenhydramine - but not enough to be statistically certain. The numbers were too close to call it a direct cause.
So why do experts still warn against them? Because real-world patterns matter. A 2023 review by the American Geriatrics Society gave first-gen antihistamines their highest risk rating: “Avoid.” Why? Because even if the risk isn’t huge for every person, it adds up. Older adults often take multiple medications. Add a daily antihistamine to a list that includes a blood pressure pill, a painkiller, and a sleep aid - and the cumulative anticholinergic burden can tip the scales.
What the Experts Really Say
Dr. Shelley Gray, who led the landmark 2015 study, puts it plainly: “The strongest signals are with antidepressants and bladder medications. Antihistamines aren’t the biggest offender - but they’re still avoidable.”On the other hand, Dr. Malaz Boustani, a dementia researcher at Indiana University, warns that even small risks matter when you’re older. “A little bit of anticholinergic activity every day for 10 years? That’s not harmless. It’s like leaving a slow leak in your car’s radiator. You don’t notice it until the engine overheats.”
The American Academy of Neurology and the Choosing Wisely campaign both agree: stop using diphenhydramine for chronic insomnia in older adults. It’s not just outdated - it’s potentially dangerous.
People Are Still Using These Drugs - And They Don’t Know Why
A 2022 survey by the National Council on Aging found that 42% of adults over 65 regularly take over-the-counter antihistamines for sleep. And 78% of them had no idea these drugs carry anticholinergic risks.Reddit threads are full of stories like this: “My mom took Benadryl every night for 15 years. Her doctor said it was fine. Now she has dementia. Was it the medicine?”
Drugs.com reviews show a split: 4.2 out of 5 stars for effectiveness, but only 2.8 for safety. Over 68% of comments mention long-term use concerns. People are sensing something’s off - even if they can’t prove it.
And here’s the kicker: many of these drugs are still sold without clear warnings. The FDA requires dementia risk labels on prescription anticholinergics - but not on over-the-counter sleep aids. In Europe, patient leaflets now include warnings about “potential long-term cognitive effects.” In the U.S.? Still just “may cause drowsiness.”
What Should You Do Instead?
If you or a loved one is taking diphenhydramine or doxylamine regularly, here’s what to do:- Check your meds. Look at the active ingredient. If it’s diphenhydramine, doxylamine, or chlorpheniramine - you’re on a first-gen antihistamine.
- Switch to a second-gen option. Try loratadine, cetirizine, or fexofenadine. They work just as well for allergies and don’t mess with your brain.
- For sleep, try non-drug options. Cognitive behavioral therapy for insomnia (CBT-I) works better than pills for older adults. Studies show 70-80% success rates. The catch? Therapists are hard to find, and Medicare pays only $85-$120 per session. But it’s worth it.
- Ask your doctor about Silenor. This prescription sleep aid (low-dose doxepin) has minimal anticholinergic effects and is approved specifically for older adults.
Don’t stop cold turkey. Talk to your pharmacist or doctor first. Suddenly quitting can cause rebound insomnia or worse.
The Bigger Picture: Why This Matters
The global market for first-gen antihistamines has dropped 24% since 2015. Sales of second-gen versions have jumped nearly 20% in the same time. That’s not just marketing - it’s people learning.Researchers are now running big new studies. The ABCO study, launched in 2023 with $4.2 million in NIH funding, is tracking 5,000 older adults for a decade. Early data from the UK Biobank suggests that when you account for underlying sleep problems, antihistamine use doesn’t raise dementia risk. That’s huge - it means the problem might not be the drug, but why you’re taking it.
Still, the safest bet? Don’t take a drug that blocks acetylcholine unless you absolutely have to. Your brain doesn’t make more of it as you age. Every pill you take that blocks it is one less tool you have to fight memory loss.
There’s no magic bullet. But there is a simple rule: if you’re over 65 and taking an OTC sleep aid or allergy pill every night, ask yourself - is this helping me, or just masking a problem? And is there a safer way?
Antihistamines aren’t poison. But for long-term use in older adults, they’re not harmless either. The evidence isn’t perfect. But the warning signs are loud enough to listen to.
Do all antihistamines increase dementia risk?
No. Only first-generation antihistamines like diphenhydramine (Benadryl), doxylamine, and chlorpheniramine have strong anticholinergic effects linked to potential cognitive risks. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have minimal to no brain penetration and are considered safe for long-term use in older adults.
Is it safe to take Benadryl occasionally?
Yes, occasional use - like once or twice a month for allergies or a bad night’s sleep - is generally safe for most people. The concern is chronic, daily use over months or years. The more often and longer you take first-gen antihistamines, the higher the potential risk to cognitive function.
What’s the safest sleep aid for older adults?
Non-drug approaches like cognitive behavioral therapy for insomnia (CBT-I) are the most effective and safest long-term option. If medication is needed, low-dose doxepin (Silenor) is approved for older adults and has minimal anticholinergic effects. Avoid diphenhydramine and doxylamine entirely for chronic sleep issues.
Can I stop taking diphenhydramine cold turkey?
It’s not recommended. Stopping suddenly after long-term use can cause rebound insomnia, anxiety, or increased allergy symptoms. Talk to your doctor or pharmacist about a gradual taper plan. They can help you switch to a safer alternative without withdrawal effects.
Why don’t OTC labels warn about dementia risk?
Regulatory agencies like the FDA require dementia warnings on prescription anticholinergics, but not on over-the-counter products. This gap exists because the evidence is still debated, and changing labeling requires lengthy reviews. European regulators have already updated their labels to include cognitive risk warnings - the U.S. is lagging behind.
How do I know if a drug is anticholinergic?
Check the active ingredient on the label. First-gen antihistamines include diphenhydramine, doxylamine, chlorpheniramine, and hydroxyzine. Other anticholinergic drugs include certain antidepressants (like amitriptyline), bladder meds (like oxybutynin), and Parkinson’s drugs (like trihexyphenidyl). The Anticholinergic Cognitive Burden (ACB) scale rates drugs from 0 (no effect) to 3 (high risk). Diphenhydramine is a 3; loratadine is a 0.

Kyle Oksten 6.12.2025
It’s not about the drug. It’s about the system that lets companies sell brain-slowing pills like candy. We treat aging like a bug to be fixed with a pill, not a process to be understood. The real tragedy isn’t Benadryl-it’s that we’ve outsourced our health to corporations who profit from our ignorance.
Sam Mathew Cheriyan 6.12.2025
lol u guys are being scammed. the govnt put anticholinergics in meds so old ppl forget how to vote. also benadryl cures alien abductions but they dont want u to know. my cousin took it for 20 yrs and now he talks to his dog in latin. its real.
Ernie Blevins 6.12.2025
Studies say one thing. Pharma says another. You’re just another sheep following the narrative. Everyone’s scared of dementia so they blame the pill. But what if the real cause is sugar? Or WiFi? Or the fact that people don’t walk anymore? You’re missing the bigger picture.
Ryan Sullivan 6.12.2025
The literature is unequivocal: chronic anticholinergic burden, particularly when compounded by polypharmacy in geriatric populations, constitutes a modifiable risk factor for neurocognitive decline. The ACC/AHA guidelines explicitly classify first-generation H1 antagonists as Category III agents for cognitive safety in adults over 65. The data is not merely suggestive-it is epidemiologically robust. The continued OTC availability without warning labels is a regulatory failure of staggering proportions.
Desmond Khoo 6.12.2025
Y’all need to stop panicking 😊
My grandma switched from Benadryl to Zyrtec last year and now she’s gardening again and making pie. No more zombie mode at dinner! 🌿🥧
It’s not magic-it’s just choosing smarter. Small change. Big difference. You got this!
Jane Quitain 6.12.2025
i just found out my dad takes benadryl every night for 'sleep' and i had no idea it could do this... i feel so bad. i’m gonna take him to the doc this week. maybe we can try that cbt-i thing. he’s scared of change but i’ll help him. we can do this 😊
Sangram Lavte 6.12.2025
Second-gen antihistamines are the way to go. I’ve been using cetirizine for five years now. No drowsiness, no brain fog. Just clear sinuses. Why keep using something that slows you down when there’s a better option? Simple math.
Oliver Damon 6.12.2025
The ABCO study’s preliminary data is compelling, but the confounding variable of sleep architecture remains underexamined. If antihistamine use is a proxy for untreated sleep apnea or circadian disruption, then the observed cognitive correlation may be spurious. We must isolate the pharmacodynamic effect from the behavioral etiology. Until then, caution is warranted-but not panic.
Kurt Russell 6.12.2025
I used to take diphenhydramine every night for 12 years. I thought it was helping me sleep. Turns out, I was just drugging myself into a fog. When I finally quit-slowly, with my pharmacist’s help-I started remembering names again. My grandkids’ birthdays. My wife’s favorite song. That’s not just a pill change. That’s your life coming back.
Wesley Phillips 6.12.2025
Oh wow another article telling old people what to do with their bodies. Next they’ll ban breathing without a prescription. Benadryl has been around since 1946. If it was dangerous, we’d all be dead by now. I’m 72 and I take it every night. I’m fine. Your fear is just marketing.
Nancy Carlsen 6.12.2025
My aunt took Zyrtec after reading this and now she’s playing piano again 🎹
She said her mind felt lighter. Like the fog lifted. It’s not about fear-it’s about giving your brain space to breathe. If you’re over 65 and still using Benadryl, please, just ask your pharmacist. One question could change everything 💛
Helen Maples 6.12.2025
Stop making excuses. If you’re taking diphenhydramine nightly, you’re not just risking dementia-you’re actively choosing a slower decline. This isn’t a debate. It’s a public health emergency. Your laziness isn’t a lifestyle. Get off the pill. Talk to your doctor. Or don’t. But don’t pretend you didn’t know.