Why Blood Pressure Control Matters for Kidney Disease
If you have kidney disease, high blood pressure isn’t just a side issue-it’s a direct threat to your kidneys. Every time your blood pressure spikes, it puts extra strain on the tiny filters in your kidneys called glomeruli. Over time, that strain leads to scarring, protein leakage into the urine, and faster loss of kidney function. The goal isn’t just to lower numbers on a monitor. It’s to slow down the damage before it’s too late.
That’s where ACE inhibitors and ARBs come in. These aren’t just regular blood pressure pills. They’re the only class of antihypertensives proven to directly protect the kidneys in people with chronic kidney disease (CKD), especially when proteinuria is present. Studies show they can cut the risk of kidney failure by up to 40% in people with diabetes or hypertension. Yet, despite decades of solid evidence, many patients still don’t get them-even when they should.
How ACE Inhibitors and ARBs Actually Work
Both ACE inhibitors and ARBs target the same system: the renin-angiotensin-aldosterone system (RAAS). This system is like a pressure regulator in your body. When it gets overactive-which often happens in kidney disease-it causes blood vessels to tighten, increases salt and water retention, and raises pressure inside the kidney’s filtering units.
ACE inhibitors, like lisinopril and enalapril, block the enzyme that turns angiotensin I into angiotensin II. Less angiotensin II means relaxed blood vessels and lower pressure. ARBs, such as losartan and valsartan, do something similar but differently: they block the receptors that angiotensin II binds to. So even if angiotensin II is still around, it can’t do its job.
The result? Lower blood pressure, less pressure inside the kidney filters, and less protein leaking into the urine. That’s the key. Protein in the urine (albuminuria) is one of the earliest signs of kidney damage-and also one of the best predictors of how fast it will worsen. Reducing that protein by 30-50% with ACE inhibitors or ARBs can literally change the course of your disease.
What the Evidence Says: Real Numbers, Real Outcomes
Let’s talk numbers, because this isn’t theory-it’s backed by data from tens of thousands of patients.
- These drugs lower systolic blood pressure by 10-15 mmHg on average-enough to make a real difference.
- They reduce urinary protein by 30-50%. In people with diabetic kidney disease, that drop can mean the difference between needing dialysis in 10 years versus 20.
- A 2024 study of 1,237 patients with advanced CKD (eGFR below 20) showed those taking ACE inhibitors or ARBs had a 34% lower risk of reaching kidney failure compared to those on other blood pressure meds.
- Meta-analyses confirm a 25% reduction in risk of ending up on dialysis or needing a transplant.
What’s surprising? These benefits hold even in late-stage kidney disease. For years, doctors were afraid to use these drugs when eGFR dropped below 30. But recent studies-including a UK trial with 3-year follow-up-show that continuing them actually helps preserve kidney function. Stopping them doesn’t help. It hurts.
ACE Inhibitors vs. ARBs: What’s the Difference?
Both work similarly. Both protect the kidneys. But they’re not identical.
ACE inhibitors are older. Captopril was the first, approved in 1981. They’re cheaper, widely available, and often first-line. But they come with a well-known side effect: a dry, nagging cough. It happens in 5-20% of users. It’s not dangerous, but it’s annoying enough that many people quit taking them.
ARBs came later, in the mid-90s. Losartan was the first. They don’t cause cough. That’s why many patients switch to ARBs when they can’t tolerate ACE inhibitors. They’re equally effective at lowering blood pressure and reducing proteinuria. No major difference in kidney protection.
There’s one other difference: angioedema. A rare but serious swelling of the face or throat. It occurs in about 0.1-0.2% of ACE inhibitor users. ARBs have even lower risk. If you’ve ever had angioedema on an ACE inhibitor, never go back.
When You Shouldn’t Use Them (And When You Should)
These drugs aren’t for everyone. But they’re for more people than you think.
**Avoid them if you have:**
- History of angioedema from an ACE inhibitor
- Severe bilateral renal artery stenosis (narrowing of kidney arteries)
- Pregnancy (they can harm the unborn baby)
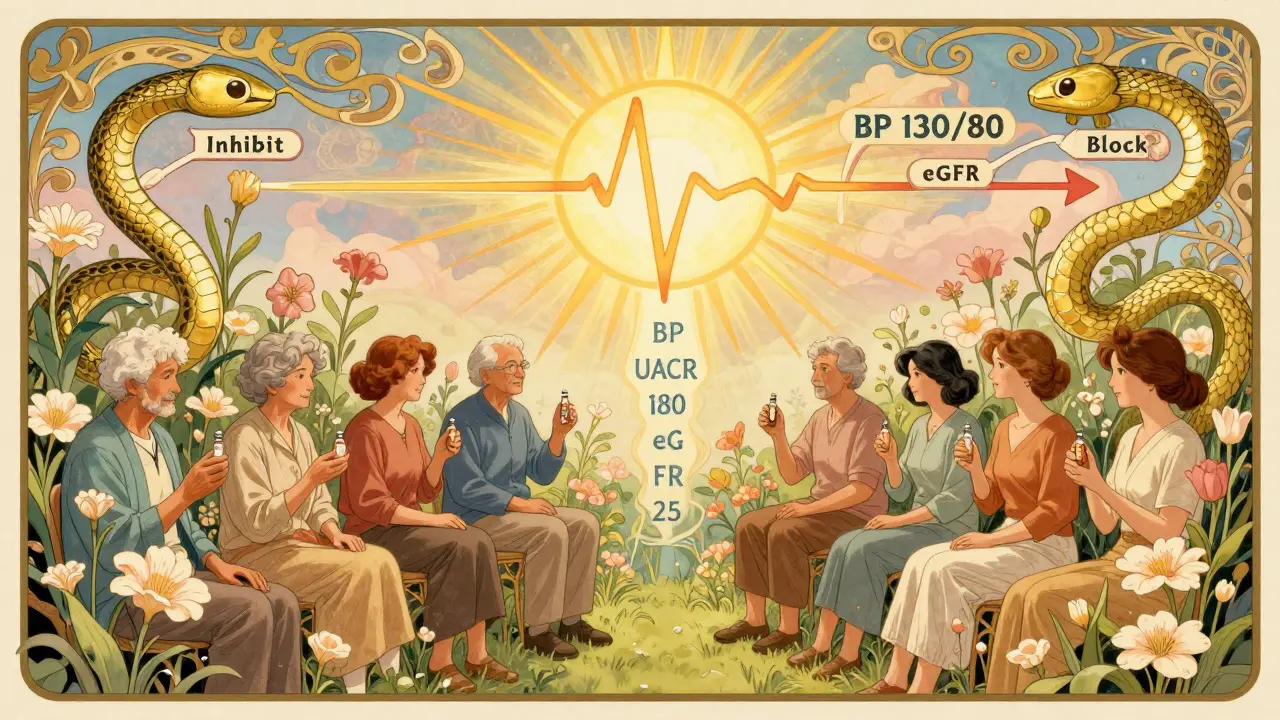
**They’re recommended for:**
- Anyone with CKD and proteinuria (UACR >200 mg/g)
- People with diabetes and kidney disease
- Those with hypertension and reduced eGFR
- Even in stage IV or V CKD-as long as potassium is below 5.0 mmol/L and eGFR is above 15 mL/min
The 2023 KDIGO guidelines are clear: don’t stop these drugs just because your kidneys are failing. In fact, continuing them may delay dialysis.
Safety Concerns: Hyperkalemia and Kidney Function Drops
The biggest fears around ACE inhibitors and ARBs are hyperkalemia (high potassium) and a sudden drop in eGFR.
Yes, about 10-15% of patients develop hyperkalemia (potassium >5.0 mmol/L). But that doesn’t mean stop the drug. It means monitor. Check potassium levels 1-2 weeks after starting or increasing the dose. If it’s above 5.5, pause the medication, adjust diet (reduce potassium-rich foods like bananas, potatoes, oranges), and retest. Often, it normalizes with simple tweaks.
As for eGFR drops: 5-10% of patients see a temporary 30%+ drop in kidney function after starting. This isn’t damage-it’s a sign the drug is working. The kidneys are relaxing their internal pressure. If the drop is more than 30% and stays high after 2 weeks, then reevaluate. But if it stabilizes? Keep going. Stopping it out of fear can accelerate kidney decline.
Why So Many People Still Don’t Get Them
Here’s the sad part: only 20-25% of eligible patients with CKD and proteinuria are on these drugs. Even in advanced disease, only 58% are getting them, compared to 82% in early-stage CKD.
Why? Fear. Misinformation. Outdated thinking.
Some doctors still believe “if your kidneys are bad, don’t use RAAS blockers.” But the data says otherwise. A 2023 review from the American Society of Nephrology called this “therapeutic nihilism”-giving up on proven treatments because of unfounded fears.
Another reason? Cost and access. In some places, ARBs are more expensive than generic ACE inhibitors. But even a low-cost lisinopril can make a life-changing difference.
What to Do If You Have Kidney Disease
If you have CKD and high blood pressure:
- Ask your doctor if you’re a candidate for an ACE inhibitor or ARB.
- Get your urine albumin-to-creatinine ratio (UACR) tested. If it’s above 200 mg/g, you’re definitely a candidate.
- Have baseline blood tests: eGFR and serum potassium.
- Start low, go slow. A low dose is fine at first.
- Check potassium and eGFR 1-2 weeks after starting.
- If you get a dry cough, don’t quit-ask about switching to an ARB.
- Don’t stop because your eGFR dips a bit. Talk to your nephrologist first.
And if you’re on dialysis or have stage 5 CKD? Still ask. Evidence now supports continuing these drugs if potassium is controlled and you’re not at risk for dangerous drops.
The Future: What’s Next Beyond ACE and ARB?
Research is moving forward. New drugs like sacubitril/valsartan (ARNI) are showing promise in reducing kidney decline in heart failure patients with CKD. One 2024 trial found it slowed kidney function loss by 22% more than enalapril alone.
But for now, ACE inhibitors and ARBs remain the gold standard. They’re affordable, well-studied, and effective. No other class of blood pressure meds offers the same level of kidney protection.
Can ACE inhibitors or ARBs cure kidney disease?
No, they don’t cure kidney disease. But they slow its progression significantly. In many cases, they can delay the need for dialysis by years-or even prevent it altogether. Their job is protection, not reversal.
I have stage 4 CKD. Should I still take an ACE inhibitor or ARB?
Yes, if your potassium is below 5.0 mmol/L and your eGFR is above 15 mL/min. Recent studies show continuing these drugs reduces the risk of kidney failure by over 30%. Stopping them doesn’t help your kidneys-it may hurt them.
What if I get a cough from lisinopril?
It’s a common side effect, affecting up to 20% of users. It’s harmless but annoying. Don’t stop the medication on your own. Ask your doctor to switch you to an ARB like losartan or valsartan. You’ll get the same kidney protection without the cough.
Can I take ACE inhibitors and ARBs together?
Generally, no. Combining them increases the risk of hyperkalemia and acute kidney injury without offering much extra benefit. The 2023 KDIGO guidelines advise against dual therapy. Stick to one, at the highest tolerated dose.
How often should I get my blood work checked?
When you start or change the dose, check potassium and eGFR within 1-2 weeks. Once stable, check every 3-6 months. More often if you’re sick, dehydrated, or on other medications like NSAIDs or diuretics.
Are ARBs better than ACE inhibitors for kidney protection?
No major difference. Both reduce proteinuria and slow kidney decline equally. ARBs have fewer side effects like cough and angioedema, so they’re often preferred if you can’t tolerate ACE inhibitors. But neither is superior for kidney protection.

