What Is Borderline Personality Disorder?
Borderline Personality Disorder (BPD) isn’t just being emotional or dramatic. It’s a real, painful condition where emotions swing wildly, relationships feel unstable, and the fear of being abandoned can trigger self-harm or suicidal thoughts. People with BPD often feel empty inside, react intensely to small triggers, and struggle to calm down once they’re upset. This isn’t weakness-it’s a neurological and psychological pattern shaped by biology, trauma, and environment. The good news? It’s treatable. And one of the most effective ways to manage it is through DBT skills.
Why DBT Works When Other Therapies Fall Short
Traditional talk therapy often fails people with BPD because it assumes they can reflect calmly on their feelings. But when someone is in emotional crisis, logic doesn’t work. That’s why Dr. Marsha Linehan created Dialectical Behavior Therapy in the late 1980s. DBT doesn’t just talk about emotions-it teaches you how to survive them. It’s built on two powerful ideas: accepting yourself as you are right now, while also changing what’s hurting you. This balance-called a dialectic-is what makes DBT unique.
Research backs this up. A major 2006 study found DBT reduced self-harm by 46% compared to standard care. Another in 2015 showed it cut suicide attempts in half over a year. The American Psychological Association gives DBT its highest rating: Level 1, meaning it has strong, repeated evidence of success. It’s not magic. It’s a skill set you learn, like riding a bike or playing piano. You get better with practice.
The Four Core DBT Skill Modules
DBT isn’t one thing-it’s four clear skill areas, each designed to tackle a different part of BPD. You don’t need to master them all at once. Start with one, then build.
Mindfulness: Ground Yourself in the Now
Mindfulness in DBT isn’t about meditation apps or chanting. It’s about noticing what’s happening without getting swept away. The goal? To stop reacting automatically and start responding intentionally. You learn three "what" skills: observe (notice your thoughts), describe (put words to them), and participate (jump into the moment fully). And three "how" skills: do it non-judgmentally (no "I’m bad for feeling this"), one-mindfully (focus on one thing at a time), and effectively (do what works, not what feels right).
One person shared on Reddit: "I used to scream at my partner over a dirty dish. Now I pause, say ‘I’m feeling overwhelmed,’ and walk away. It’s not perfect-but it’s progress." Studies show just 8 weeks of mindfulness practice boosts emotional regulation by 32% in people with BPD.
Distress Tolerance: Get Through the Crisis Without Self-Destruction
When you’re in a full-blown emotional meltdown-heart racing, thoughts of self-harm swirling-logic vanishes. That’s where distress tolerance skills come in. These aren’t about fixing the problem. They’re about surviving it.
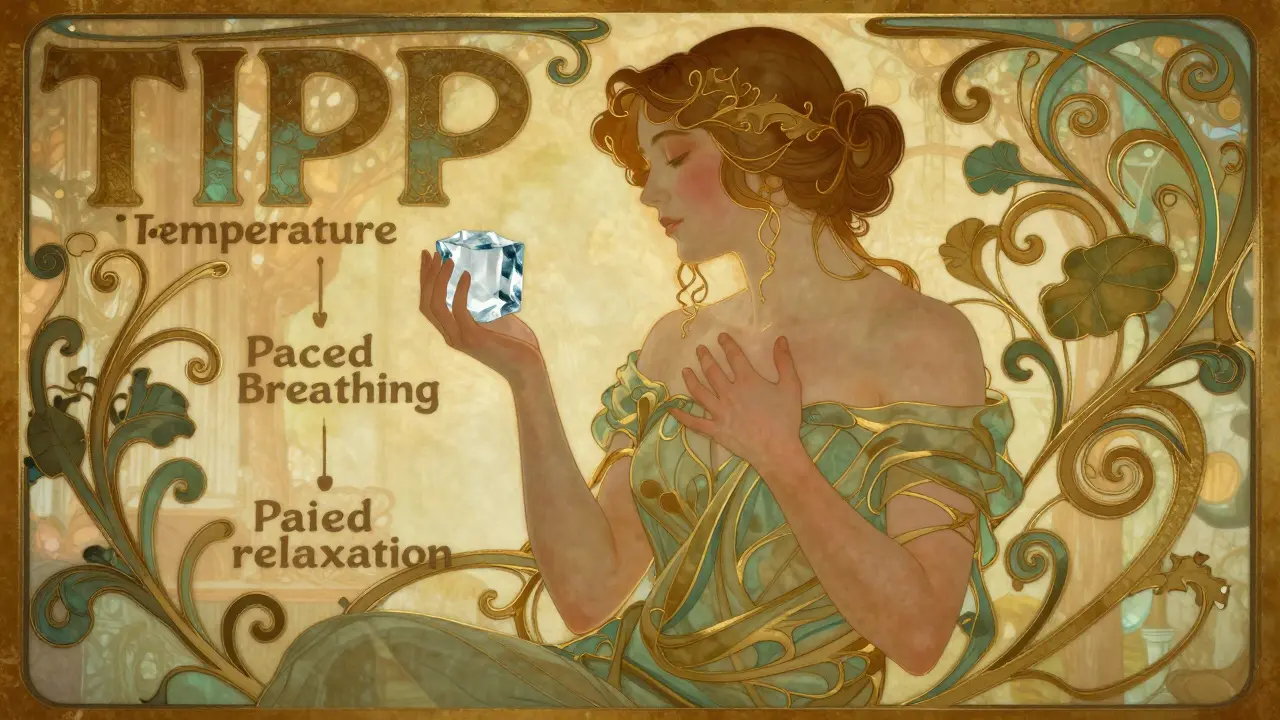
One of the most used tools is TIPP:
- Temperature: Splash ice water on your face or hold an ice cube. This triggers your body’s dive reflex and instantly calms your nervous system.
- Intense exercise: Run in place, do 20 jumping jacks. Burn off the adrenaline.
- Paced breathing: Breathe in for 4 seconds, hold for 4, out for 6. Slows your heart rate.
- Paired muscle relaxation: Tense your fists for 5 seconds, then release. Do this through your whole body.
Other tools include ACCEPTS (distract with activities, helping others, or watching a funny video) and IMPROVE (imagine a safe place, find meaning, pray, relax, focus on one thing, take a mini-vacation, give yourself encouragement). A 2019 study showed these skills cut ER visits for self-harm by 57% in the first four months.
Emotion Regulation: Stop Being Controlled by Your Feelings
People with BPD often feel emotions like they’re on fire-intense, fast, and impossible to turn off. Emotion regulation skills teach you how to cool them down before they burn you.
PLEASE is a simple acronym for physical care:
- Physical illness: Treat medical issues. Pain makes emotions worse.
- Lbalanced eating: Skip meals? You’ll feel more irritable.
- Evoid mood-altering drugs: Alcohol, weed, pills-they don’t fix anything.
- Abalanced sleep: Sleep deprivation = emotional chaos.
- Sexercise: Even a 10-minute walk lowers stress hormones.
Then there’s ABC: Accumulate positive emotions (watch your favorite movie, call a friend), Build mastery (do something you’re good at), and Cope ahead (plan for hard situations before they happen). One user said: "I started writing down three good things every night. After two months, I didn’t feel so alone anymore."
Interpersonal Effectiveness: Say What You Need Without Losing Yourself
Relationships are the biggest trigger for people with BPD. You want connection, but fear rejection. You say things in anger, then regret them. DBT gives you clear scripts.
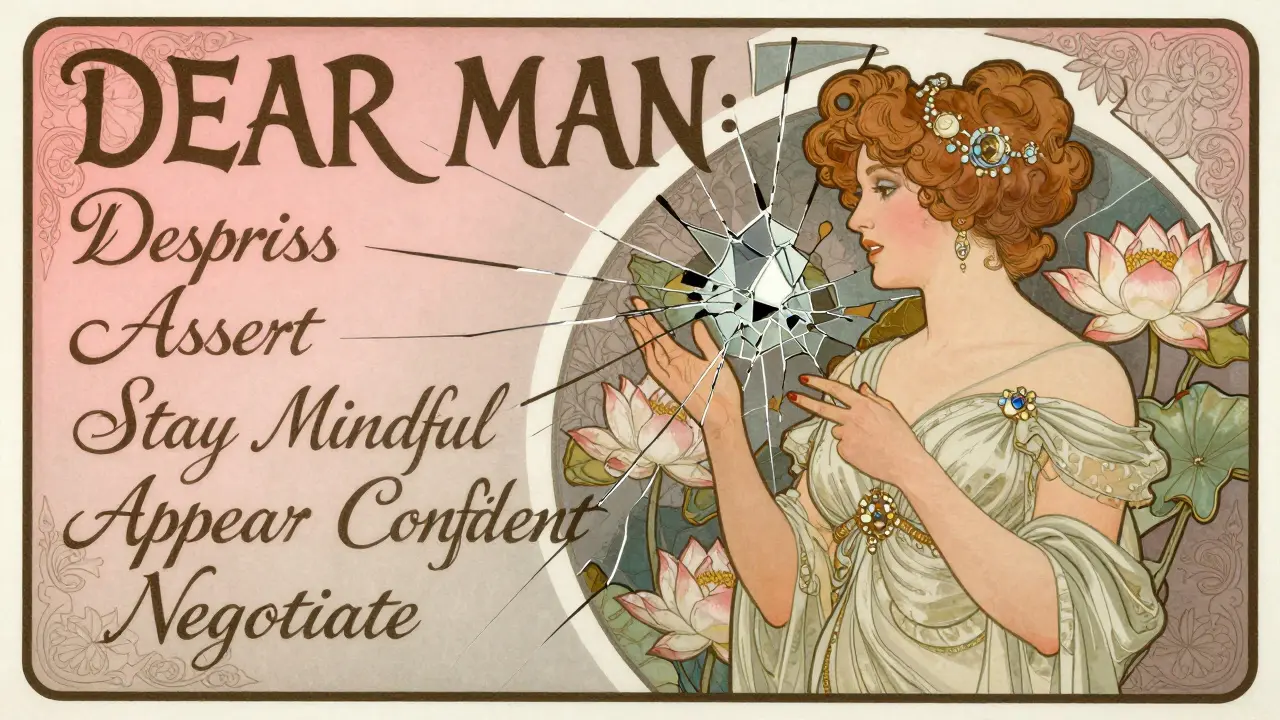
DEAR MAN helps you ask for what you need:
- Describe the situation ("When you canceled our plans last minute...")
- Express how you feel ("I felt hurt and ignored")
- Assert your need ("I need you to text me if you’re running late")
- Reinforce ("It would mean a lot to me if we could stick to plans")
- Stay Mindful (don’t get distracted by their reaction)
- Appear confident (even if you’re scared)
- Negotiate (be willing to compromise)
GIVE keeps relationships healthy: Be Gentle, show Interest, Validate their feelings, use an Easy manner. FAST helps you stay true to yourself: be Fair, no Apologies (for your needs), Stick to your values, be Truthful. A 2023 study found these skills improved relationship satisfaction by 28%.
Crisis Planning: Your Personal Emergency Kit
DBT doesn’t wait for crisis to strike-it prepares you for it. A crisis plan is a written, personalized guide you keep on your phone, in your wallet, or taped to your mirror. It includes:
- Your top 3 distress tolerance skills (TIPP, IMPROVE, etc.)
- People you can call (therapist, friend, crisis line)
- Safe places to go (a quiet room, a park, a friend’s house)
- Reasons you want to live (write them down: "I want to see my niece graduate," "I want to finish my art")
- What to do if you feel like harming yourself (call 988, go to ER, text a crisis text line)
One person wrote: "My crisis plan has a photo of my dog. When I’m in the dark, I look at it and remember I’m not alone."
How to Start DBT: What to Expect
Getting started isn’t easy. Most comprehensive DBT programs require:
- Weekly 1-hour individual therapy
- Weekly 2-hour skills group
- 24/7 phone coaching (you can call your therapist during a crisis)
- Homework (skills worksheets, emotion logs)
The whole program usually lasts 6 to 12 months. It’s a commitment-but it’s not forever. Many people say the first month is the hardest. Emotions feel louder. Homework feels overwhelming. But by month 6, skills start sticking. One user said: "I used to cry for hours after an argument. Now I use Paced Breathing. It doesn’t fix everything-but it stops me from breaking down."
DBT vs. Other Treatments
There are other therapies for BPD. But DBT stands out.
Mentalization-Based Therapy (MBT) helps you understand others’ minds-but doesn’t give you crisis tools. Schema Therapy digs into childhood wounds-but takes longer. STEPPS is a group program that works well for symptoms but not for acute crises.
DBT wins because it gives you real, usable tools you can apply in the moment. It’s not about understanding why you feel this way. It’s about what to do right now.
But it’s not perfect. Some people find the structure too rigid. Others struggle with the time commitment. And not every therapist is trained in true DBT. Look for someone certified by the Linehan Institute. As of 2023, there are only about 1,842 certified DBT therapists worldwide.

Real Stories: What Works-and What Doesn’t
Reddit’s r/BPD and r/DBT communities are full of raw, honest stories.
"I used DEAR MAN to tell my mom I needed space. I didn’t yell. I didn’t cry. I said, ‘I love you, but I need to take a break.’ She cried. Then she said, ‘I’m sorry I made you feel this way.’ That never happened before."
"I tried DBT for 4 months. I hated the worksheets. I quit. Then I downloaded the DBT Coach app. I used TIPP when I felt suicidal. I didn’t self-harm that night. I went back to therapy."
"My therapist made me feel like I was broken. My new one says, ‘Your feelings make sense. Now let’s find a better way to handle them.’ That changed everything."
Barriers and Solutions
DBT isn’t easy to access. Only 35% of U.S. clinics offer full DBT. In rural areas, it’s under 12%. Insurance often covers only 12-20 sessions a year. Therapy costs can be high.
But things are changing. Telehealth has boosted access by 28% since 2020. Apps like DBT Coach and Virtual Reality DBT are helping people practice skills at home. A 2023 study showed 68% of users stuck with app-based DBT, compared to just 45% with paper worksheets.
If you can’t find a DBT program, start with the skills. Buy the DBT Skills Training Workbook. Use free resources from the Linehan Institute. Practice one skill every day. You don’t need a therapist to begin healing.
What’s Next for DBT?
DBT is evolving. In 2023, the Linehan Institute launched a new "DBT-Crisis Survival" certification. Researchers are testing AI tools that adjust skill recommendations based on your heart rate or voice tone. The goal? Make DBT more personal, more responsive, more accessible.
But the core hasn’t changed. It’s still about learning to live with intense emotions-not fighting them, not hiding from them, not being ashamed of them. It’s about building a life worth staying for.
Can you do DBT on your own without a therapist?
Yes, you can start using DBT skills on your own. Many people begin by reading the DBT Skills Training Workbook or using apps like DBT Coach. You can learn mindfulness, distress tolerance, and emotion regulation techniques without a therapist. But full DBT includes group sessions, phone coaching, and therapist feedback-elements that significantly boost success rates. If you’re in crisis, struggling with self-harm, or feel overwhelmed, working with a certified DBT therapist is strongly recommended.
How long does it take to see results from DBT?
Most people notice small improvements within 2-4 weeks, like using a skill during a moment of distress. Meaningful changes-like fewer self-harm episodes, better relationships, or less emotional flooding-usually take 6-8 months of consistent practice. Studies show that by month 6, skill use becomes more automatic. It’s not a quick fix, but the results last.
Is DBT only for people who self-harm?
No. While DBT was originally designed for people with chronic self-harm and suicidal thoughts, it works for anyone struggling with emotional overwhelm, intense relationships, or impulsive reactions. Many people without a BPD diagnosis use DBT skills to manage anxiety, depression, trauma, or even workplace stress. The tools are universal.
What if I can’t afford DBT therapy?
Cost is a real barrier. But options exist. Look for community mental health centers that offer sliding-scale fees. Some universities train DBT therapists and offer low-cost services. Online groups and free worksheets from the Linehan Institute can help you start. Apps like DBT Coach and MindShift cost less than $10/month. You don’t need a full program to benefit-start with one skill, practice it daily, and build from there.
Can DBT help with anger issues?
Yes. Anger in BPD is often a response to feeling abandoned or misunderstood. DBT’s Emotion Regulation module teaches you to identify anger triggers, reduce vulnerability (through PLEASE), and use Opposite Action-doing the opposite of what your anger urges you to do. Instead of yelling, you might walk away. Instead of smashing something, you might squeeze a stress ball. These skills reduce the intensity and frequency of angry outbursts.
Do DBT skills work for teens?
Absolutely. DBT has been adapted for adolescents and is now one of the most effective treatments for teens with BPD symptoms, self-harm, or emotional outbursts. The skills are simplified, and family involvement is often included. Studies show teens using DBT have fewer hospitalizations and improved school performance. The core principles-acceptance and change-resonate with young people who feel misunderstood.
What’s the difference between DBT and CBT?
CBT (Cognitive Behavioral Therapy) focuses on changing negative thoughts. DBT adds acceptance, mindfulness, and crisis skills. CBT might help you reframe "I’m worthless" to "I’m having a hard time right now." DBT says: "Your feeling makes sense. Now let’s get through this moment without hurting yourself." DBT is more action-focused in crisis, while CBT is more thought-focused. For BPD, DBT is more effective because it addresses the intense emotional pain that CBT alone can’t reach.
Is DBT covered by insurance?
Most private insurers and Medicare cover DBT when it’s delivered as a full program by a certified provider. Coverage usually includes 12-20 sessions per year for BPD. Check with your provider about requirements-some need a formal diagnosis and proof of medical necessity. Phone coaching and group sessions may have separate coverage rules. Always ask your therapist’s office to verify benefits before starting.
Can DBT help with trauma?
Yes, but not directly. DBT doesn’t focus on processing past trauma like EMDR or trauma-focused CBT. However, it builds the emotional stability and distress tolerance needed to safely explore trauma later. Many therapists use DBT first to stabilize clients, then add trauma work. If you’re in active crisis or have severe dissociation, DBT helps you get grounded before diving into trauma memories.
What if I’m not ready for DBT?
You don’t have to be "ready." DBT meets you where you are. Many people start because they’re desperate, not because they’re motivated. That’s okay. Start small. Try one skill for one day. Use TIPP when you feel overwhelmed. Write down one reason you want to live. You don’t need to believe in it to benefit from it. Action often comes before motivation.

Cara Hritz 21.12.2025
i think dbt is great but honestly the worksheets are so boring i quit after 2 weeks. then i found the dbt coach app and it was like a whole new world. ice cube trick saved me like 3x last month. also why does everyone say 'you need a therapist' like its the only way? i'm not rich but i'm alive and that counts.
ps: typo: 'dive reflext' should be 'dive reflex' lol
Kiranjit Kaur 21.12.2025
OMG YES 😭 I used TIPP when my boss canceled my vacation last minute and I was about to scream into a pillow. Ice cube. Jumping jacks. Paced breathing. I didn't quit my job. I didn't cry in the elevator. I just... breathed. And now I have a little sticky note on my mirror: "Breathe first, react later." DBT isn't magic, it's just... practical love for your brain. 🌱💖
Sai Keerthan Reddy Proddatoori 21.12.2025
this is all western nonsense. in india we dont need apps or worksheets. we just pray, work hard, and suffer in silence. why do you need to talk about feelings? emotions are weakness. if you cant handle life, dont have kids. this dbt stuff is just therapy capitalism. waste of time.
Johnnie R. Bailey 21.12.2025
There’s something deeply human about the way DBT refuses to pathologize pain. It doesn’t say, 'You're broken.' It says, 'You're overwhelmed, and here’s how to hold yourself together.' That distinction? That’s the difference between healing and humiliation. I’ve seen people go from crisis to calm not because they 'got better'-but because they finally learned how to be with their own storms. And honestly? That’s the most radical act of self-respect I’ve ever witnessed.
Tony Du bled 21.12.2025
I tried DBT after my third ER visit. Didn't believe in it. Thought it was just another fad. Then I used paced breathing during a panic attack while waiting in line for coffee. Didn't even know I was doing it until I realized I wasn't hyperventilating. Now I do it without thinking. No apps. No worksheets. Just breath. That's all.
Art Van Gelder 21.12.2025
Let me tell you something most people don’t say out loud: DBT doesn’t fix you. It doesn’t make you 'normal.' What it does is give you a lifeline when you’re drowning in your own mind. I used to think if I could just understand why I felt this way, I’d be okay. But understanding doesn’t stop the scream inside your chest. What stops it? The ice cube. The walk around the block. The text to your friend that says 'I’m not okay.' It’s not about enlightenment. It’s about survival. And the fact that we’ve built a system where you have to fight for access to these tools? That’s the real tragedy. Not the disorder. The system.
Ajay Brahmandam 21.12.2025
I'm from India and I started using DBT skills after reading this post. Used TIPP when my brother yelled at me for not getting married. Ice water, 10 squats, slow breath. Didn't cry. Didn't yell back. Just said 'I need space.' He didn't get it, but I did. DBT isn't just for BPD. It's for anyone who feels too much. And yeah, it works even without a therapist.
jenny guachamboza 21.12.2025
okay but who funded this? is this a pharma ad? why is everyone so obsessed with 'skills' like we're robots? emotions aren't bugs to be fixed. also i saw a video of a therapist crying in a dbt group and i think it's all just performative trauma tourism. and btw 'dive reflext' is spelled wrong again. lol.
Tarun Sharma 21.12.2025
The approach described is methodical and grounded in empirical evidence. It is commendable that structured interventions such as DBT have demonstrated efficacy in reducing self-harm and improving interpersonal functioning. However, cultural adaptation remains essential for global applicability.
Aliyu Sani 21.12.2025
yo i been usin DBT skills since my cousin died. TIPP saved me when i was in the hospital waitin for the docs. Ice cube on my neck? yeah. Paced breath? yeah. I ain't got no therapist but i got the app and my homie who texts me 'u good?' when i ghost for 2 days. this ain't therapy, this is survival. and i ain't ashamed of it.
Jim Brown 21.12.2025
There is a profound metaphysical humility in DBT’s core dialectic: to accept what is, while simultaneously striving to change what can be. This is not cognitive behavioral engineering-it is the ancient art of holding paradox, rendered in modern clinical language. The person who says, 'I look at my dog and remember I’m not alone,' has articulated a truth older than any therapy: that connection, however small, is the antidote to existential void. We do not heal by fixing ourselves. We heal by remembering we are not meant to be alone.
Jamison Kissh 21.12.2025
I wonder if the reason DBT works is because it doesn't try to change the person's emotional wiring-it just gives them tools to navigate it. Like teaching someone with poor eyesight to wear glasses instead of trying to 'fix' their retinas. The brain isn't broken. It's just operating in a high-stress environment with no manual. DBT is the manual. And honestly? We should all have one.
Kathryn Weymouth 21.12.2025
I’ve been using DBT for nine months. I didn’t know I had BPD until I read this post. The crisis plan I made? I keep it in my phone case. The photo of my sister holding my newborn? That’s the one I look at. I didn’t need a therapist to start. I just needed to believe I deserved to survive. And now I do.