When your doctor orders a brain MRI, it’s not because they’re being overly cautious-it’s because they need to see what’s happening inside your skull in a way no other test can. Unlike X-rays or CT scans, MRI doesn’t use radiation. Instead, it uses strong magnets and radio waves to create incredibly detailed pictures of your brain’s soft tissues. This makes it the best tool for spotting problems like tiny strokes, early signs of multiple sclerosis, or even small tumors that other scans might miss. If you’ve ever wondered what those black-and-white images actually mean, here’s what you need to know.
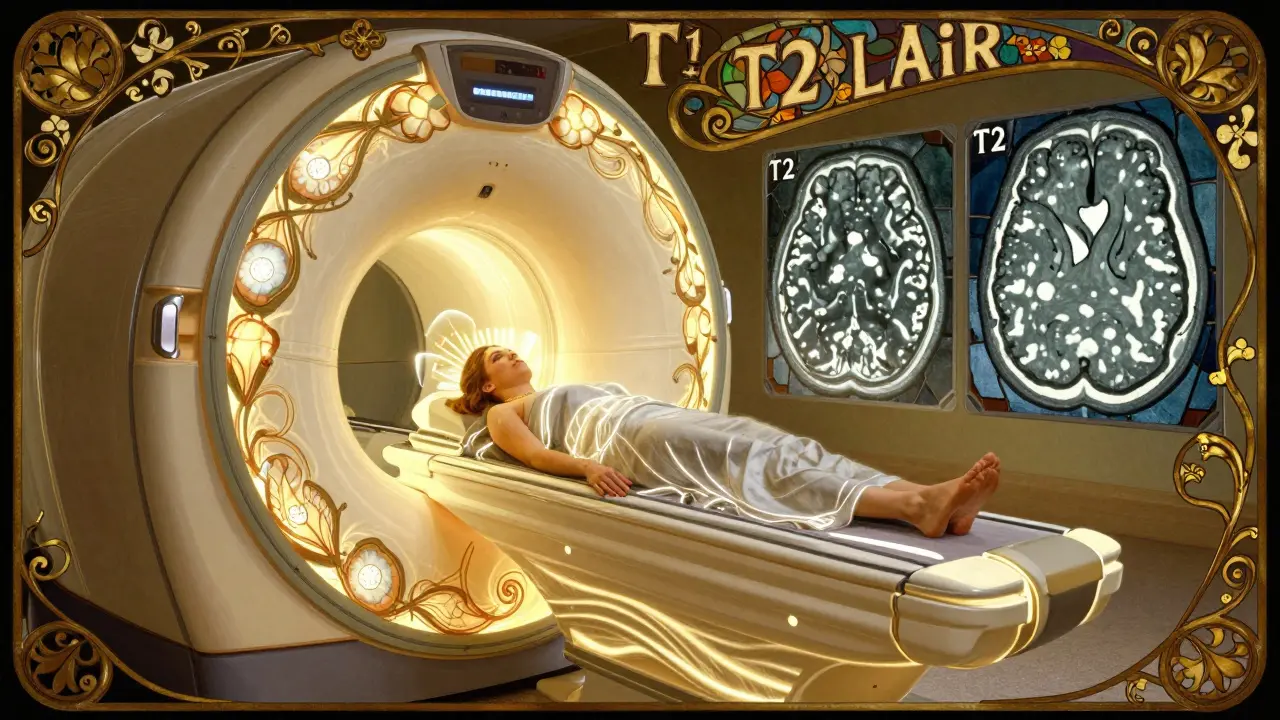
What Happens During a Brain MRI?
You’ll lie on a table that slides into a long, narrow tube. The machine makes loud knocking noises-like a jackhammer inside a metal drum-as it switches magnetic fields on and off. It’s not painful, but it can feel claustrophobic. Most scans take between 30 and 45 minutes. You need to stay still. Even a small movement can blur the images, making them harder to read.
Before you go in, you’ll be asked about metal implants. Pacemakers, cochlear implants, and some older aneurysm clips can be dangerous near the magnet. Even some tattoos contain metal that can heat up. If you’re unsure, bring a list of your medical devices. The staff will check if it’s safe.
You won’t feel the magnetic field, but you might feel warm in your head. That’s normal. Some people get a contrast dye injected through an IV to make certain abnormalities stand out more clearly. It’s not always needed, but when it is, it helps show inflammation, tumors, or active MS plaques.
The Three Key MRI Sequences You Need to Know
Brain MRI doesn’t take just one picture. It takes several, each highlighting different tissues. Three sequences are most important for diagnosis: T1-weighted, T2-weighted, and FLAIR.
T1-weighted images show anatomy best. Fat and some types of tissue look bright white. Cerebrospinal fluid (CSF)-the liquid that surrounds your brain and spinal cord-looks dark. This sequence is great for seeing the shape of your brain, the size of your ventricles, and whether there’s any swelling or mass effect pushing structures out of place.
T2-weighted images make water shine. Anything with extra fluid-like swelling from a stroke, infection, or tumor-shows up bright. But here’s the catch: CSF is also bright on T2. That means if you’re looking at a spot near the ventricles, it’s hard to tell if the brightness is from a lesion or just fluid. That’s where FLAIR comes in.
FLAIR (Fluid-Attenuated Inversion Recovery) is like T2, but with one big tweak: it turns CSF dark. This makes it easier to spot brain lesions that sit right next to fluid-filled spaces. If you see bright spots around the ventricles on FLAIR, that’s often a sign of multiple sclerosis. On T2, those same spots might look like normal fluid.
Doctors look at all three together. A lesion that’s bright on T2 and FLAIR but dark on T1 is typically an old or chronic injury. If it’s bright on all three, it might be something active-like an infection or a growing tumor.
Common Findings on Brain MRI
Not every bright spot means something serious. Many findings are normal-or at least common-with age.
White matter hyperintensities are small bright spots, often near the ventricles. They’re seen in 15% of people under 50 and up to 90% of those over 70. These are usually tiny blood vessel changes from aging, high blood pressure, or diabetes. They’re not always linked to symptoms, but if they’re widespread, they can increase stroke risk.
Small lacunar infarcts are tiny areas of dead brain tissue from blocked blood vessels. They’re often found in the deep parts of the brain-like the basal ganglia or thalamus. These might have happened years ago and never caused noticeable symptoms. But if you’ve had a stroke before, finding more of these suggests your blood vessels are still at risk.
Multiple sclerosis plaques look like bright spots on FLAIR, often near the ventricles, in the brainstem, or along the spinal cord. They’re usually oval-shaped and perpendicular to the ventricles-a pattern called “Dawson’s fingers.” These aren’t scars from injury; they’re areas where the immune system has attacked the protective coating around nerves. Tracking these over time helps doctors decide if treatment is working.
Acute stroke shows up fast on a special sequence called diffusion-weighted imaging (DWI). Within minutes of a stroke, water movement in brain cells gets blocked. DWI picks that up immediately. If the apparent diffusion coefficient (ADC) is below 600 x 10^-6 mm²/s, it’s a clear sign of new damage. This is why MRI is preferred over CT for stroke diagnosis-it catches changes hours before CT can.
Brain tumors vary in appearance. Some are clearly defined masses with swelling around them. Others blend in. Contrast dye helps here. If a tumor lights up after the dye is injected, it means the blood-brain barrier is broken-often a sign of an aggressive tumor. Benign tumors like meningiomas often have a clear border and may push on nearby structures without invading them.
Microbleeds are tiny spots of old bleeding, seen on sequences like SWI or gradient echo. They’re common in older adults with high blood pressure or amyloid buildup (linked to Alzheimer’s). Finding more than five microbleeds increases stroke risk and can change how doctors treat blood thinners.
When Is MRI Overused?
Not every headache needs an MRI. In fact, for people with typical migraines and no neurological symptoms, MRI is rarely helpful. Studies show that only about 1.3% of brain MRIs done for routine headaches reveal something serious-like a tumor or aneurysm. The American College of Radiology says MRI is “usually not appropriate” for uncomplicated migraines.
Doctors should look for red flags before ordering: sudden severe headache (like a thunderclap), new weakness, vision loss, seizures, confusion, or changes in personality. If none of those are present, the chance of finding something dangerous is extremely low. Unnecessary MRIs lead to false alarms-finding harmless spots that cause anxiety and lead to more tests.
How MRI Compares to CT
CT scans are faster-often done in under five minutes. That’s why they’re the first choice in trauma or suspected stroke when time is critical. CT can quickly show a large bleed or fracture. But it misses a lot.
CT can’t see small strokes in the brainstem or early MS plaques. It also can’t distinguish between old and new damage well. And it uses radiation-something you don’t want repeated over time, especially in younger patients.
MRIs give you 30-40 different shades of gray, compared to CT’s 4-5. That’s why MRI sees subtle differences in brain tissue. It’s also the only way to reliably detect small tumors like acoustic neuromas under 3mm in size.
But MRI has downsides. It’s slower, louder, and more expensive. A brain MRI costs $1,200 to $3,500 in the U.S., while a CT runs $500 to $1,500. And not every hospital has one-only 76% of U.S. hospitals have MRI machines, compared to 98% with CT.
What Comes Next After the Scan?
After your MRI, a radiologist reviews the images. They’ll look for patterns: where are the lesions? Are they symmetric? Do they match known disease patterns? Then they send a report to your doctor.
Your doctor won’t just look at the images-they’ll combine them with your symptoms, medical history, and maybe blood tests or EEG results. A bright spot on MRI doesn’t mean you have MS. It could be a sign of high blood pressure, a past infection, or even just aging.
If something unusual is found, you might need follow-up scans. For MS, doctors often repeat MRIs every 6-12 months to see if new lesions are forming. For tumors, they might monitor size over time. The goal isn’t just to find something-it’s to understand if it’s changing, growing, or stable.
What’s New in Brain MRI?
Technology keeps improving. Ultra-high-field 7.0T MRI machines are now in a few academic centers. They can show brain layers as thin as 0.5mm-something impossible with standard machines. These are still research tools, but they may one day help diagnose Alzheimer’s before symptoms start.
Artificial intelligence is also making scans faster. Some software can cut scan time in half without losing detail. AI can even highlight areas that look suspicious, helping radiologists catch small lesions they might miss.
Quantitative MRI is another frontier. Instead of just saying “there’s a bright spot,” new techniques measure actual changes in tissue-like how much water is in a lesion, or how fast blood flows through it. These measurements could one day replace guesswork with numbers, making diagnosis more precise.
For now, though, the basics still matter most. Knowing how to read T1, T2, and FLAIR sequences, understanding what’s normal with age, and recognizing when something is truly abnormal-that’s what saves lives.
Can a brain MRI detect Alzheimer’s disease?
A standard brain MRI can’t diagnose Alzheimer’s directly, but it can show signs that support the diagnosis. People with Alzheimer’s often have shrinkage in the hippocampus and other memory-related areas. MRI also rules out other causes of dementia, like tumors, strokes, or normal pressure hydrocephalus. Newer techniques, like amyloid PET scans combined with MRI, are becoming more common in research centers, but they’re not yet routine in most clinics.
Why do I need to stay still during an MRI?
MRI works by detecting tiny changes in how hydrogen atoms in your body respond to magnetic pulses. Even a small movement-like swallowing or shifting your head-can blur the images. Blurry images make it harder for radiologists to spot small lesions, especially those under 5mm. Staying still ensures the scan is clear and accurate, reducing the chance of needing a repeat scan.
Are MRI findings always serious?
No. Many people have bright spots on their brain MRI that mean nothing. White matter hyperintensities are common with aging and high blood pressure. Small old strokes (lacunar infarcts) often cause no symptoms. Even incidental tumors, like small meningiomas, can be harmless and never need treatment. The key is context: your symptoms, age, and medical history determine if a finding matters.
Can MRI show if a stroke is recent or old?
Yes, especially with diffusion-weighted imaging (DWI). Acute strokes show up bright on DWI within minutes and stay visible for about a week. Older strokes don’t light up on DWI but may appear as dark areas on T1 or FLAIR. Radiologists use this pattern to tell if a stroke happened hours ago or years ago. This is critical for deciding whether to give clot-busting drugs.
Do I need contrast dye for every brain MRI?
No. Many brain MRIs are done without contrast. It’s only used when doctors suspect tumors, infections, or active inflammation like MS flare-ups. Contrast helps highlight areas where the blood-brain barrier is broken. If your scan is for headaches, memory issues, or routine monitoring of MS, contrast isn’t always needed. Your doctor will decide based on your symptoms and history.
What to Do If Your MRI Shows Something
Don’t panic. Finding an abnormality on an MRI is common. Most are not emergencies. The next step is always to talk to your doctor-not Google. Ask: Is this new? Is it growing? Does it match my symptoms? Do I need treatment, or just monitoring?
If you’re told you have MS, a small tumor, or silent strokes, ask for a copy of your images. Get a second opinion if you’re unsure. Neurologists and neuroradiologists specialize in this. Don’t accept a diagnosis based on a single scan without context.
And remember: MRI doesn’t replace clinical judgment. It’s a tool. The best diagnosis comes from combining what the scan shows with what you’re actually experiencing.