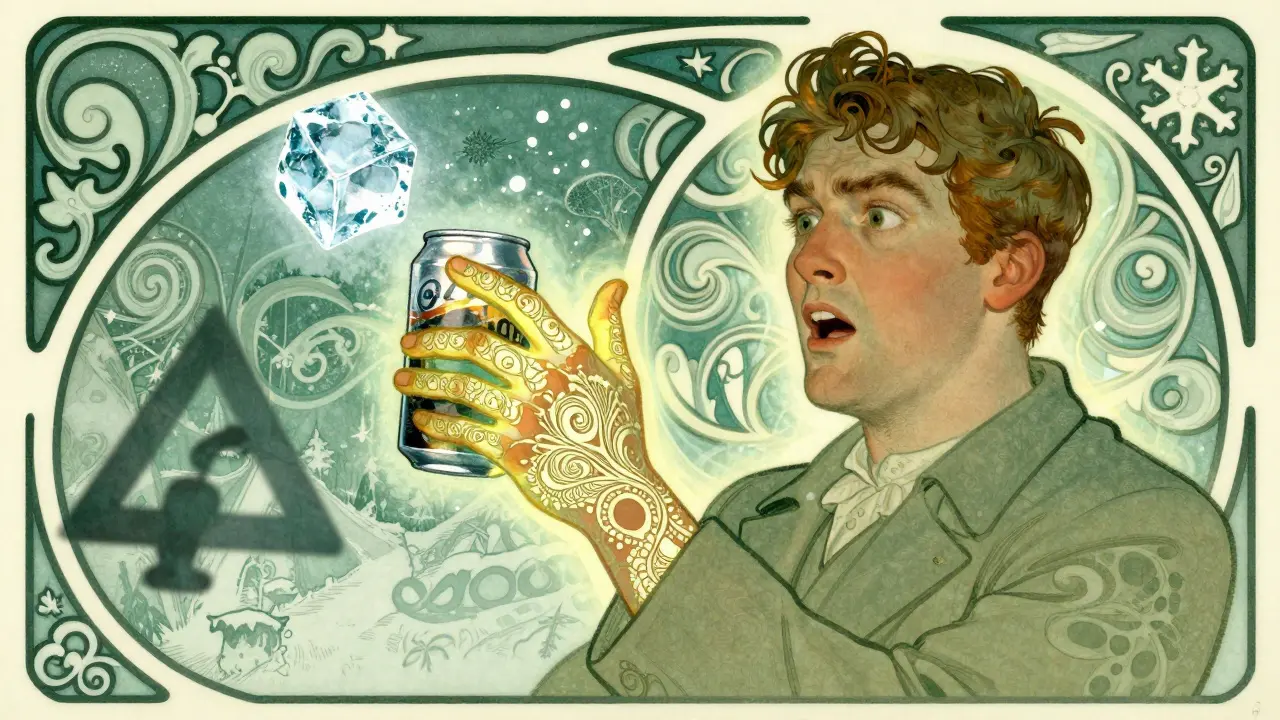
Imagine stepping into a cold shower, reaching for an ice-cold soda, or swimming in a lake - and within minutes, your skin breaks out in angry, itchy welts. Not from an infection. Not from a food you ate. Just from the cold. This isn’t just discomfort. For some people, it’s a medical condition called cold-induced urticaria - a type of allergic reaction triggered by cold temperatures.
It sounds strange. How can cold, something we all experience daily, cause an allergic response? The answer lies in how your immune system misreads cold as a threat. When skin is exposed to temperatures below a certain threshold - sometimes as warm as 20°C (68°F) - mast cells in the skin release histamine and other chemicals. That’s what causes the red, swollen, itchy hives. The reaction doesn’t happen while you’re still cold. It kicks in during rewarming. That’s why people often feel the worst symptoms right after coming inside from the cold.
Who Gets Cold-Induced Urticaria?
This condition is rare. Studies estimate only about 0.05% of the population has it. But that still means thousands of people are affected. It most often starts between ages 18 and 25, though it can appear at any age. In 95% of cases, there’s no known cause - it just shows up. These are called idiopathic cases. In the other 5%, it’s linked to something else: infections like hepatitis or mononucleosis, insect bites (especially ladybugs, oddly enough), blood cancers, or inherited conditions.
There are different types. Some people only get hives on their hands when they hold a cold drink. Others break out all over after swimming in cool water. A few have a rare inherited form called familial cold autoinflammatory syndrome (FCAS), which causes fever, joint pain, and hives after cold exposure - and needs completely different treatment than the usual kind.
What Does It Look Like?
The symptoms are clear and predictable:
- Itchy, red welts (hives) on skin exposed to cold
- Swelling of the lips or tongue after eating cold food or drinking chilled beverages
- Swollen hands after holding something cold - reported in 78% of cases
- Lightheadedness, dizziness, or fainting if a large area of skin reacts
- Headaches, rapid heartbeat, or wheezing in severe cases
The most dangerous scenario? Swimming in cold water. When a big portion of your body is exposed, the reaction can be systemic. Blood pressure can drop. Swelling can block airways. There are documented cases of drowning because someone suddenly couldn’t move or breathe after entering cold water. That’s why this isn’t just a nuisance - it can be life-threatening.
How Is It Diagnosed?
Doctors don’t guess. They test. The standard method is the ice cube test. An ice cube is placed on the forearm for 1 to 5 minutes. If a raised, red, itchy welt forms within 10 minutes - especially as the skin warms up - that’s a positive result. This test is 98% accurate for acquired cold urticaria.
Doctors may also ask you to keep a symptom diary. When did the hives happen? What was the temperature? How long did they last? This helps identify your personal cold threshold. Some people react at 20°C. Others need ice water. Knowing your limit matters.
Blood tests aren’t always needed, but if your doctor suspects an underlying cause - like an infection or cancer - they might check for cryoglobulins, autoimmune markers, or other signs.
Treatment: From Antihistamines to Emergency Gear
There’s no cure - but there are ways to control it.
First-line treatment: Non-sedating antihistamines. These include cetirizine (Zyrtec), loratadine (Claritin), and desloratadine (Clarinex). Most people start with the standard dose. But for cold urticaria, doctors often increase the dose - up to four times higher than usual. So instead of 10mg of cetirizine, you might take 40mg daily. This is safe and approved by international guidelines. About 50-60% of patients see big improvement at this level.
If antihistamines don’t work well enough, there’s another option: omalizumab (Xolair). This is an injection originally for asthma, but it’s now FDA-approved for chronic hives. In studies, it helped 60-70% of cold urticaria patients who didn’t respond to antihistamines. It works by blocking the IgE antibody that triggers mast cell release.
For those with severe reactions, carrying an epinephrine autoinjector (like an EpiPen) is essential. Your doctor will teach you how and when to use it - especially before swimming, skiing, or any activity where cold exposure is likely. Don’t wait until you’re in trouble. Have it ready.
There’s also a newer drug called berotralstat (Orladeyo), approved for hereditary angioedema. A 2023 clinical trial showed it reduced cold urticaria symptoms by 58% in people who didn’t respond to omalizumab. It’s not yet widely used for this condition, but it’s a promising option for tough cases.
Living With It: Practical Tips That Work
Medication helps - but behavior changes save lives.
- Avoid ice-cold drinks and foods. Even a sip of iced tea or a bite of ice cream can trigger lip swelling. Stick to room-temperature or warm options.
- Test before you swim. Dip one hand in the water for 5 minutes. If you get a reaction, don’t go in. This simple step prevents 85% of aquatic emergencies.
- Dress smart. Layer up. Wear moisture-wicking base layers under your coat. Wet skin reacts worse. Keeping dry reduces reactions by 60-70%.
- Use a cold alert device. Wearable sensors like the Cold Alert sensor can notify you when ambient temperature drops below your personal threshold. In a 2022 trial, they were 92% accurate.
- Use apps. The Urticaria Tracker app lets you log symptoms and temperature. Users report 30% better control because they spot patterns - like how a 15°C day triggers hives, but 18°C doesn’t.
- Never swim alone. Always have someone nearby who knows your condition and how to use an EpiPen.
If you’re having surgery or a medical procedure, tell your anesthesiologist. Cold IV fluids or a chilly operating room can trigger a reaction. Hospitals now have guidelines requiring warming blankets and room temperatures above 21°C (70°F) for CU patients.

What About Cold Desensitization?
Some people try to train their body to tolerate cold. It’s called desensitization. The idea? Take regular cold showers, gradually lowering the temperature over weeks. A few patients report success. But studies show 40% drop out because it’s too uncomfortable. And there’s a risk - one wrong step, and you could trigger a full-body reaction. It’s not recommended without medical supervision.
Will It Go Away?
Good news: many people outgrow it. The European Urticaria Registry found that 35% of patients experience spontaneous remission within five years. If your symptoms started suddenly - say, after an infection - you’re more likely to recover than if it’s been going on for years. In familial cases, it’s usually lifelong.
What’s on the Horizon?
Research is moving fast. Trials are testing low-dose naltrexone (a drug used for autoimmune conditions) and new cold desensitization protocols. One study showed 70% adherence in the first 12 weeks. Genetic research has identified mutations in the PLCG2 gene linked to familial cold urticaria - and drugs like anakinra (Kineret) are helping those patients by blocking the inflammation at its source.
What’s clear? Cold-induced urticaria is more than just hives. It’s a complex immune response with real risks. But with the right diagnosis, treatment, and habits, most people live full, active lives - without fear of the cold.
Can cold-induced urticaria be cured?
There is no known cure for cold-induced urticaria, but many people experience spontaneous remission within 5 years. Treatment focuses on managing symptoms with antihistamines, epinephrine for emergencies, and lifestyle adjustments. In rare inherited forms, targeted therapies like anakinra can control the condition effectively.
Is cold urticaria the same as frostbite?
No. Frostbite is tissue damage from freezing, causing numbness, blistering, and cell death. Cold urticaria is an allergic reaction - the skin doesn’t freeze. Instead, mast cells release histamine, causing hives and swelling. One is physical injury; the other is immune overreaction.
Can you develop cold urticaria later in life?
Yes. While it most often starts between ages 18 and 25, it can appear at any age. Cases have been documented in people over 60, sometimes following infections like hepatitis or after exposure to certain insect bites. Late-onset cases are often linked to underlying medical conditions.
Why do hives appear after rewarming, not during cold exposure?
The exact reason isn’t fully understood, but it’s tied to how blood flow changes. When skin cools, blood vessels constrict. When it warms up again, blood rushes back, triggering mast cells to release histamine. This surge of fluid and chemicals causes swelling and itching - which is why the worst symptoms happen after you come inside from the cold.
Are antihistamines safe at higher doses for cold urticaria?
Yes. International guidelines support increasing doses of second-generation antihistamines like cetirizine up to four times the standard dose (e.g., 40mg daily) for chronic urticaria. Studies show this is safe and effective for most patients. Side effects like drowsiness are rare with non-sedating types, but always follow your doctor’s guidance.
Can you outgrow cold-induced urticaria?
Yes. About 35% of patients experience spontaneous remission within five years. Those with sudden onset after an infection are more likely to recover than those with long-standing, chronic symptoms. Familial forms, however, are usually lifelong.
Is swimming dangerous with cold urticaria?
Extremely dangerous. Cold water immersion is the most common cause of life-threatening reactions, including anaphylaxis and drowning. Even if you’ve swum before without issues, a drop in water temperature or longer exposure can trigger a full-body reaction. Always test with one hand first, never swim alone, and carry an EpiPen.
What should you do if you have a severe reaction?
Use your epinephrine autoinjector immediately if you experience dizziness, difficulty breathing, swelling of the throat, or a rapid drop in blood pressure. Call emergency services right away. Even if symptoms improve, you still need medical evaluation - a second wave of reaction can occur hours later.
Can cold urticaria be passed down genetically?
Yes, but rarely. Familial cold autoinflammatory syndrome (FCAS) is an inherited condition caused by mutations in genes like PLCG2. It causes hives, fever, and joint pain after cold exposure and typically starts in childhood. It requires different treatment than typical cold urticaria, often involving interleukin-1 inhibitors like anakinra.
Do temperature sensors really help people with cold urticaria?
Yes. Wearable devices like the Cold Alert sensor, tested in a 2022 multicenter trial, showed 92% accuracy in predicting reactions below individual temperature thresholds. Users report fewer flare-ups because they get alerts before exposure - helping them avoid triggers proactively.

Alex Ogle 7.02.2026
So I’ve had this since I was 19. No family history. No infections. Just… one day, holding a frozen juice box, my hand turned into a balloon. Not even cold enough to make you shiver. Just… cold. Took me three years to get diagnosed because doctors thought I was allergic to something in the packaging. The ice cube test? Yeah. It’s brutal. But accurate. Now I carry two EpiPens in my coat pockets. One for the car, one for my bag. You learn to live with it. But you never forget how terrifying it feels when your throat starts closing after a walk outside in October. It’s not ‘just hives.’ It’s a silent grenade in your immune system.
And yeah, the 40mg of Zyrtec? Works like magic. I used to think I was crazy for taking that much. Turns out, doctors have been telling people to do this for years. Just nobody told me.
Also - never trust a doctor who says ‘it’ll go away.’ Mine did. I’m 31 now. Still here. Still careful.
Lyle Whyatt 7.02.2026
Just wanted to say - the Cold Alert sensor? I got one last winter. Game-changer. I’ve got mine synced to my phone and my smart thermostat. When it hits 17°C, my house automatically turns up the heat and sends me a vibration. I didn’t even know I was reacting to drafts until I started tracking. My flare-ups dropped by 80%.
Also, the app Urticaria Tracker? Use it. I logged every single episode for six months. Found out I react to cold air moving across my skin - not just temperature. So now I wear a neck gaiter indoors in winter. Sounds ridiculous, but it works. Small changes, big difference.
And yeah, swimming alone? No. Ever. I have a buddy who’s trained in EpiPen use. We have a signal: if I grab my neck and look panicked? He knows. No words needed. That’s life-saving stuff.
MANI V 7.02.2026
Oh, so now we’re medicalizing discomfort? People used to just… deal with the cold. Now we need wearable sensors, apps, and four-times-dose antihistamines? This is what happens when society turns every minor inconvenience into a ‘condition.’
I’ve lived in three countries. Ice water? Cold showers? I’ve done it all. No hives. No drama. Maybe if you stopped being so sensitive - literally and figuratively - you wouldn’t need all this tech. It’s not a disease. It’s a lack of toughness.
And don’t get me started on the ‘epinephrine for a cold drink’ crowd. Next thing you know, people will need oxygen tanks for walking into air-conditioned malls.
Susan Kwan 7.02.2026
Wow. So the solution to ‘I get hives from cold’ is… more drugs, more gadgets, and more fear? Congrats, medicine. You turned a weird quirk into a full-blown survival manual.
Let me guess - next they’ll sell a ‘Cold Urticaria Survival Kit’ with a $300 hoodie, a Bluetooth ice cube, and a therapist who specializes in ‘cold trauma.’
Meanwhile, people who actually have real autoimmune disorders are still waiting for insurance coverage. But hey - at least your hives come with a mobile app and a 92% accurate sensor. You’re doing great. 🎉
Random Guy 7.02.2026
so like… i just got hives from my AC once and thought i was dying?? like why does this happen?? i thought cold = numbness, not… balloon skin??
also why is everyone carrying epipens like they’re in a zombie apocalypse?? i need to know if i’m next 😭
Tasha Lake 7.02.2026
Can we talk about the IgE pathway here? The fact that cold exposure triggers mast cell degranulation via IgE-mediated pathways is fascinating - it’s not a classic Type I hypersensitivity like peanuts or pollen, because there’s no allergen. It’s an autoallergen - the cold itself acts as the trigger. That’s why antihistamines help - they block H1 receptors - but omalizumab works because it targets the upstream IgE.
And the PLCG2 mutation in FCAS? That’s a gain-of-function mutation in phospholipase C gamma 2. It leads to constitutive inflammasome activation. That’s why anakinra (IL-1Ra) works - it interrupts the IL-1β cascade. It’s not just ‘hives’ - it’s a systemic autoinflammatory disorder in familial cases.
Also - the rewarming phenomenon? It’s likely due to transient receptor potential (TRP) channel activation, especially TRPM8 and TRPA1, which are cold-sensitive ion channels that trigger neurogenic inflammation. The rush of blood during rewarming causes localized hypoxia, which further activates mast cells. It’s a perfect storm.
Andy Cortez 7.02.2026
Yeah right. ‘Cold-induced urticaria.’ Like it’s some new fad. I’ve been cold my whole life. Never had hives. You people are just overreacting. Literally.
And these ‘cold alert devices’? That’s just capitalism turning your body into a data point. Next thing you know, your fridge will send you a notification: ‘WARNING: Milk is at 3°C. Possible hive trigger detected.’
Also - ‘don’t swim alone’? What, you’re not allowed to take a dip unless you’ve got a personal assistant with an EpiPen? That’s not living. That’s existing in a bubble. I say - embrace the cold. Build tolerance. Stop treating your skin like a fragile porcelain doll.
Jacob den Hollander 7.02.2026
Hey - just wanted to say thank you for writing this. I was diagnosed last year after a trip to Lake Tahoe. I didn’t know what was happening. Thought I was having an allergic reaction to lake water. Turned out, it was the 12°C water. I almost passed out. My wife had to drag me out.
Since then, I’ve started using the tracker app, wear thermal layers under everything, and I carry my EpiPen in my hat now (yes, really - it’s easier to reach than in a pocket).
To anyone reading this who’s scared: you’re not alone. I used to cry before winter. Now I just plan. And I’ve got a support group on Reddit. We share tips. We laugh. We survive. It’s not perfect. But it’s manageable. And you’re stronger than you think.
Also - if you’re reading this and you have this? Please, please, please - tell your doctor about the 4x antihistamine dose. Most don’t know. I had to research it myself.
Andrew Jackson 7.02.2026
It is deeply troubling that modern medicine has reduced human resilience to the level of a laboratory specimen. To prescribe four times the standard dosage of pharmaceuticals - to arm citizens with autoinjectors - to monitor ambient temperature with electronic devices - this is not healing. This is surrender.
Our ancestors braved blizzards without antihistamines. They swam in icy rivers without sensors. They did not cower before the elements - they mastered them. To treat cold as a pathogen is to misunderstand the very nature of human endurance.
Let us not mistake discomfort for disease. Let us not confuse caution with cowardice. The body is not a fragile machine to be calibrated - it is a temple of fortitude. And if one’s skin reacts to cold - perhaps the fault lies not in nature, but in the weakening of the spirit.
PAUL MCQUEEN 7.02.2026
So… this is a thing? I thought it was just people being dramatic. Like, ‘oh my skin is itchy because I touched a freezer.’
And you’re telling me some people need to carry a needle because they drank iced tea? That’s insane. Why not just… not drink iced tea?
Also - ‘familial cold autoinflammatory syndrome’? Sounds like a made-up term for people who hate winter. I’m skeptical. Where’s the peer-reviewed data? I didn’t see any links.
Kathryn Lenn 7.02.2026
Of course this is real. But have you ever wondered… who benefits? The pharmaceutical companies? The wearable tech startups? The doctors who get paid for ‘specialized consultations’?
I’ve been reading about this since 2019. There’s a pattern: first, they label a normal reaction as a disease. Then they create a ‘treatment protocol.’ Then they sell you the gear. Then they patent the sensor. Then they get FDA approval for ‘off-label’ use. It’s a loop.
And the ‘spontaneous remission’ stat? 35%? That’s the placebo effect. They don’t test that. They just assume it’s the body healing. But what if it’s just… people stopped stressing about it?
And why is there no mention of EMF sensitivity? Or glyphosate? Or 5G? Just saying.
Chima Ifeanyi 7.02.2026
Let’s analyze this from a systems biology perspective. Cold-induced urticaria is not a ‘condition’ - it’s a failure of thermoregulatory-immune crosstalk. The mast cell is a dual-sensor: it responds to both chemical and thermal stimuli. In susceptible individuals, cold exposure triggers a calcium flux via TRP channels, which synergizes with IgE-FcεRI signaling. This creates a hyper-reactive state. The rewarming phase amplifies it via NO synthase activation and endothelial shear stress.
The 40mg cetirizine protocol? It’s not ‘off-label’ - it’s evidence-based. The 2021 EAACI guidelines explicitly endorse it. But here’s the kicker: the real innovation isn’t the drug - it’s the behavioral tracking. The app logs micro-environmental triggers. That’s predictive analytics applied to immunology.
And FCAS? It’s not ‘rare.’ It’s underdiagnosed. Most cases are misclassified as fibromyalgia or chronic fatigue. The PLCG2 mutation is autosomal dominant. If you have a parent with unexplained fevers + hives since childhood - you’re at 50% risk. Genetic screening should be routine.
Alex Ogle 7.02.2026
Andy - you’re right. I did stop stressing. And that’s when the hives stopped. Not because I ‘got tough.’ But because I stopped fighting it. I stopped trying to be ‘normal.’ I stopped hiding my EpiPen. I started telling people. And suddenly - I wasn’t alone. The sensor? It’s not about fear. It’s about freedom. I can now go hiking. I can take my kid to the pool. I can live.
And yeah - I still get weird looks. But I don’t care anymore.
Thanks for the reply. You’re not wrong. You’re just… not me.