What corticosteroids actually do in autoimmune diseases
When your immune system turns on your own body, things go wrong fast. In autoimmune diseases like lupus, rheumatoid arthritis, or vasculitis, your white blood cells attack healthy tissue - causing swelling, pain, and damage. That’s where corticosteroids come in. These aren’t the same as the steroids athletes abuse. Corticosteroids are synthetic versions of cortisol, the hormone your adrenal glands make naturally to handle stress and control inflammation. They work fast. Like, hours fast. While drugs like methotrexate take weeks to show results, corticosteroids like prednisone or methylprednisolone can calm an overactive immune system in just a day or two.
They don’t cure the disease. But they stop the fire. Corticosteroids block the genes that make inflammatory proteins - the ones that trigger swelling, redness, and tissue damage. They silence signals like tumor necrosis factor-alpha and interleukins. They shut down enzymes like cyclooxygenase-2 and phospholipase A2, which are behind the pain and heat you feel in inflamed joints or skin. This isn’t guesswork. It’s science backed by decades of research from labs at Johns Hopkins, the Mayo Clinic, and peer-reviewed journals like Frontiers in Immunology.
Why doctors reach for corticosteroids first
Imagine you’re in the ER with sudden kidney failure from vasculitis. Your kidneys are being attacked by your own immune system. Time matters. Waiting for slow-acting drugs to kick in could mean permanent damage or dialysis. That’s why corticosteroids are the first line of defense. In Australia, doctors follow guidelines from the Australian Prescriber that recommend starting with 1-2 mg of prednisone per kilogram of body weight for severe cases. For life-threatening conditions like Goodpasture’s syndrome or rapidly progressive glomerulonephritis, high-dose intravenous methylprednisolone pulses are used - often alongside drugs like cyclophosphamide.
It’s not just about kidneys. In severe lupus flares, corticosteroids can stop brain inflammation. In myasthenia gravis, they help restore muscle strength. In psoriasis or inflammatory bowel disease, they reduce skin lesions and gut ulcers. The reason they’re so widely used isn’t just effectiveness - it’s speed. No other class of drug matches how quickly they turn down inflammation. That’s why, despite the risks, they remain the go-to for acute flare-ups across dozens of autoimmune conditions.
Where corticosteroids don’t work - and why
Not every autoimmune disease responds. In fact, there are four where corticosteroids offer little to no benefit: advanced type 1 diabetes, Hashimoto’s thyroiditis, Graves’ disease, and late-stage primary biliary cholangitis. Why? Because by the time these diseases reach that stage, the damage is done. The insulin-producing cells in your pancreas are already gone. The thyroid tissue is destroyed. The bile ducts in your liver are scarred. No amount of anti-inflammatory power can bring them back.
But here’s the nuance: early-stage type 1 diabetes or early primary biliary cholangitis - where some cells are still alive - might respond to short-term immunosuppression. That’s why timing matters. If you catch it early, corticosteroids can slow the attack. If you wait too long, they’re useless. This isn’t a one-size-fits-all treatment. It’s a precision tool. Doctors don’t just prescribe them because they’re powerful. They prescribe them because they know exactly when they’ll help - and when they won’t.

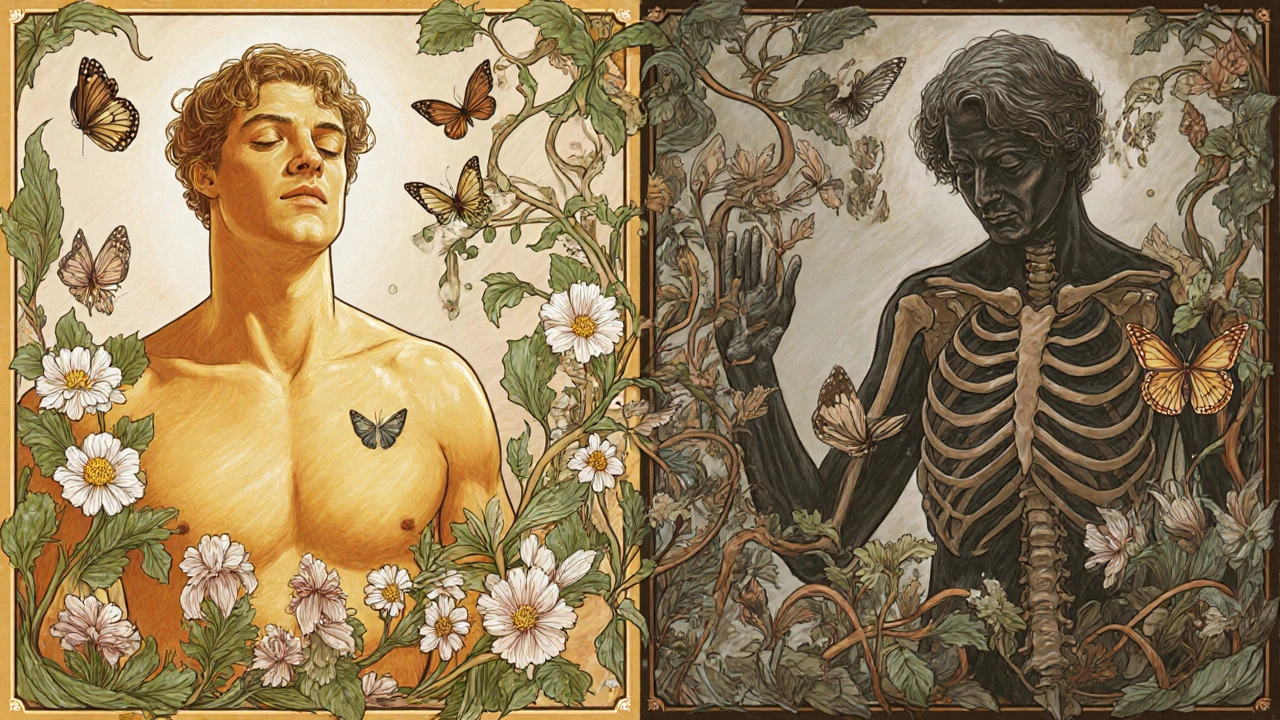
The hidden cost: long-term side effects
Using corticosteroids for more than a few weeks changes your body. The longer you take them, the more your body forgets how to make its own cortisol. This is called HPA axis suppression. If you suddenly stop, your body can’t respond to stress - and that can be deadly. That’s why you never quit cold turkey. You taper slowly, under medical supervision.
Then there’s bone loss. Up to 40% of people on long-term corticosteroids develop osteoporosis. Your bones thin out. A simple fall can break a hip. That’s why doctors prescribe calcium, vitamin D, and sometimes bisphosphonates alongside steroids. Cataracts are another common problem - cloudy lenses that blur vision. You might not notice it until you’re driving at night and everything looks hazy.
Other risks? Weight gain, especially around the face and belly. High blood sugar - even in people without diabetes. Mood swings, trouble sleeping, skin that bruises easily. Some people develop acne or dark patches on their skin. And yes, you become more sensitive to sunlight. Sunscreen isn’t optional anymore. These aren’t rare side effects. They’re expected. That’s why the Australian Prescriber and Mayo Clinic both say: use the lowest dose for the shortest time possible.
How to reduce the risks - and still get relief
The goal isn’t to avoid corticosteroids. It’s to use them smarter. The best approach now is combination therapy. Instead of relying on high-dose prednisone for months, doctors pair it with other drugs that do the heavy lifting over time. Azathioprine, methotrexate, or mycophenolate help reduce the steroid dose. This cuts side effects without losing control of the disease.
Even better: biologics. Drugs like rituximab (which targets B cells) have shown better long-term results than steroids alone in conditions like autoimmune hemolytic anemia. In some cases, rituximab is now used as a first-line treatment. The Frontiers in Immunology study showed patients on rituximab plus steroids had fewer relapses and stayed in remission longer than those on steroids alone.
Topical versions help too. For asthma or allergic rhinitis, inhaled or nasal steroids deliver the drug right where it’s needed - with far less impact on the rest of your body. For skin rashes, creams work better than pills. The key is targeting the inflammation without flooding your system.
What patients need to know before starting
If your doctor prescribes corticosteroids, ask these questions:
- What’s the goal? Are we trying to stop a flare, or manage long-term disease?
- What’s the lowest dose that will work? Can we start low and go higher if needed?
- What other drugs will I take with this to reduce steroid use?
- How will we monitor for side effects? Bone scans? Blood sugar checks? Eye exams?
- What’s the plan for stopping? How slowly will we taper?
Keep a symptom diary. Note changes in mood, weight, sleep, or joint pain. Bring it to every appointment. If you’re on steroids for more than three weeks, never skip a dose without talking to your doctor. And if you ever need emergency surgery or get seriously ill - tell every healthcare provider you’re on steroids. Your body needs that extra cortisol to survive stress.
The future: smarter steroid use
Researchers are working on ways to keep the benefits without the damage. One promising area is GILZ - a protein that mediates corticosteroid’s anti-inflammatory effects. If scientists can create a drug that mimics GILZ, we might get the same relief without the side effects. It’s still early, but it’s the kind of innovation that could change the game.
For now, corticosteroids remain the most powerful anti-inflammatory tools we have. They’ve saved lives since the 1940s. But they’re not a long-term solution. The future of autoimmune care isn’t about bigger doses - it’s about smarter combinations. Using steroids to buy time, then replacing them with targeted therapies that don’t wreck your bones, your blood sugar, or your sleep.


Shivam Goel 24.11.2025
Corticosteroids are a double-edged sword-yes, they silence cytokines like TNF-alpha and IL-6 within hours, but that HPA axis suppression? It’s not a glitch, it’s a feature of long-term use. And don’t get me started on the osteoporosis risk-40% of patients? That’s not a side effect, that’s a public health crisis waiting to happen. I’ve seen patients on 20mg prednisone for 18 months lose three vertebrae. No one talks about this enough.
Andrew McAfee 24.11.2025
I live in the US and my rheumatologist put me on prednisone for a lupus flare and I was shocked at how fast it worked but also how fast I gained weight like my face turned into a moon and I couldnt sleep and my skin felt like tissue paper and honestly I just wanted to cry every night but at least I could walk again so I guess its worth it
Elise Lakey 24.11.2025
I appreciate how the article breaks down the timing aspect-early intervention matters so much. I was diagnosed with early-stage PBC last year and my doctor was hesitant at first but after a few months of low-dose steroids plus UDCA, my liver enzymes improved. It’s not a cure but it bought me time. Thank you for highlighting that nuance.
Sharley Agarwal 24.11.2025
Everyone acts like steroids are magic. They’re not. They’re just a bandaid on a severed artery. And then you pay for it with your bones your sleep your sanity. I’m 32 and I already have cataracts from 3 years of prednisone. Don’t romanticize this.
Srikanth BH 24.11.2025
I know it sounds cliché but you’re not alone. I’ve been on steroids for 7 years with RA and yes it’s rough-but I’ve also learned to take calcium, do weight training, and never skip my taper. It’s hard but doable. And if you pair it with methotrexate? Life changes. You can still travel, work, laugh. It’s not perfect but it’s not the end either.
Kimberley Chronicle 24.11.2025
The GILZ-mediated pathway is indeed a compelling frontier-recent murine models suggest selective glucocorticoid receptor modulators (SGRMs) can dissociate transrepression from transactivation, potentially decoupling anti-inflammatory efficacy from metabolic dysregulation. If we can pharmacologically replicate this, we may finally move beyond the cortisol mimicry paradigm.
Shirou Spade 24.11.2025
It’s funny how we treat inflammation like an enemy to be crushed. But what if it’s just our body screaming for balance? Corticosteroids don’t fix the root-they just silence the scream. And silence doesn’t heal. It just makes you forget you’re bleeding. Maybe we need to ask not how to suppress more, but why the immune system turned on us in the first place.
Lisa Odence 24.11.2025
I am a clinical pharmacist with 18 years of experience and I must say that the information presented here is not only accurate but also remarkably comprehensive. The inclusion of specific dosing guidelines from the Australian Prescriber and the mention of cyclophosphamide pulses for Goodpasture’s syndrome demonstrates a high level of medical literacy. I am also pleased to see the emphasis on tapering protocols and HPA axis suppression-these are often overlooked in lay literature. 👏👏👏
Agastya Shukla 24.11.2025
The biologics angle is critical. Rituximab isn’t just an alternative-it’s a paradigm shift. In autoimmune hemolytic anemia, the relapse rate drops from 60% on steroids alone to under 20% with rituximab combo. The cost is steep, but when you factor in hospitalizations, bone fractures, and diabetes management from long-term steroids? The ROI is clear. We’re moving from suppression to redirection.
Leisha Haynes 24.11.2025
So we’re supposed to be grateful that steroids let us walk again while we gain 50 pounds and turn into a diabetic with cataracts? Cool. Cool cool cool. I’ll just keep my prednisone and my sadness and my broken hip and call it a win
Jefriady Dahri 24.11.2025
Hey everyone-just wanted to say if you're on steroids, please don't ignore your eye exams. I didn't think I needed one until I couldn't read my phone at night. Turns out I had early cataracts. Got them fixed. Life changed. Also, if you're tapering, write down how you feel every day. It helps your doc adjust better. You got this 💪
Ellen Sales 24.11.2025
I lost my job because I couldn’t stop crying on prednisone. I lost my marriage because I was too tired to be a partner. I lost my bones. And now? I’m told to ‘be grateful’ because I can still breathe. But what kind of life is that? This isn’t medicine-it’s a hostage negotiation with your own body.
Josh Zubkoff 24.11.2025
Look, I read this whole thing and honestly? It’s just a glorified drug ad. They mention the risks but bury them in paragraphs. No one’s talking about how 70% of patients on long-term steroids develop metabolic syndrome. Or how the FDA has warned about psychiatric adverse events-depression, psychosis, even suicide. And yet here we are, treating this like it’s just a minor inconvenience. Someone needs to call this out for what it is: a chemical crutch with a side of devastation.
Rachel Villegas 24.11.2025
I’ve been on low-dose prednisone for 5 years for polymyalgia. I take calcium, I do yoga, I sleep 8 hours, and I never skip my taper. It’s not perfect, but it’s the best tool we have right now. I’m alive. I can hug my grandkids. That’s worth something.