Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these aren’t accidents-they’re preventable. Whether you’re taking one pill a day or managing five different medications, getting it right isn’t optional. It’s life-or-death. The good news? You don’t need a medical degree to stay safe. Just five clear, simple rules can cut your risk dramatically.
Rule 1: Know Exactly What You’re Taking
Don’t assume the pill looks the same as last time. Medications can change shape, color, or size between refills-even if the name hasn’t changed. A 2023 ISMP report found that 12% of medication errors happen because patients didn’t notice the difference in their pills. That’s why you should always check the label and compare the pill to the description on the bottle. If it looks wrong, call your pharmacy. Don’t take it.Also, know the difference between brand and generic names. Your doctor might prescribe metoprolol, but the bottle says Lopressor. Or worse, you might get metformin instead of metoprolol-two completely different drugs that sound alike. Hospitals use “Tall Man lettering” (like METOPROLOL vs. METFORMIN) to avoid this. At home, write both names down. Keep a list. Update it every time something changes.
Rule 2: Take It at the Right Time
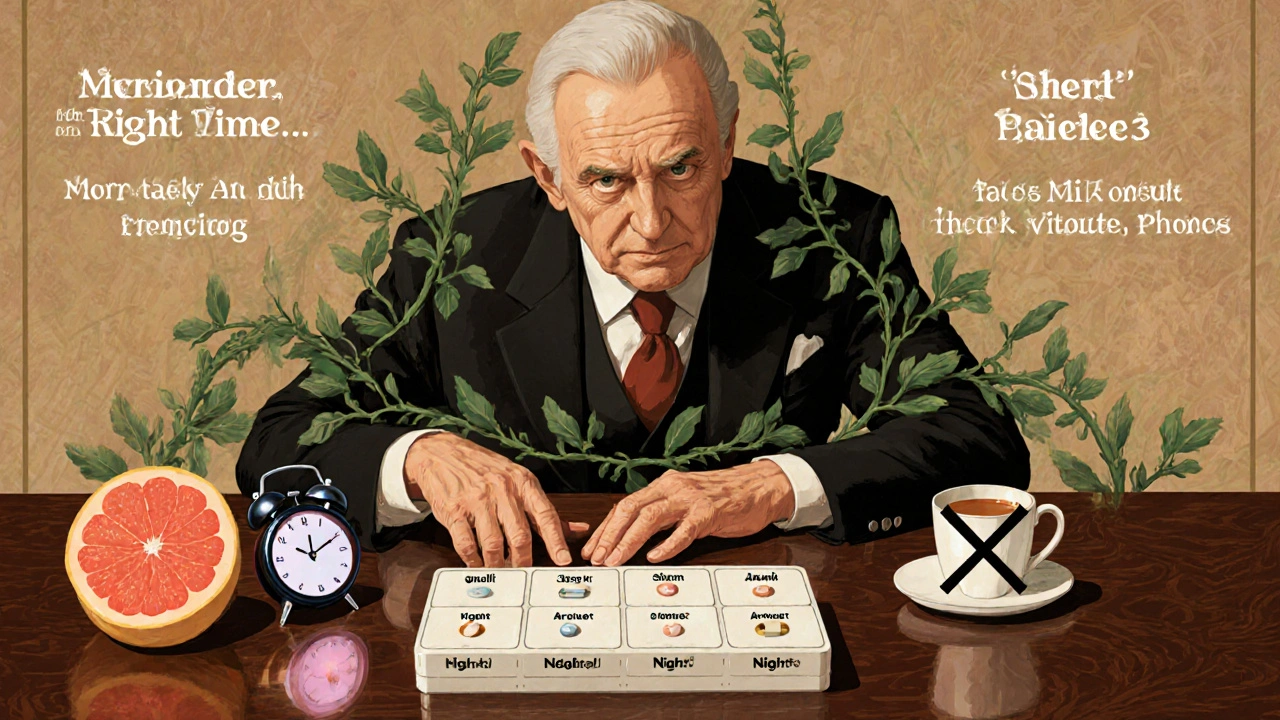
Timing matters more than you think. Some medications need to be taken on an empty stomach. Others must be spaced exactly 12 hours apart. For drugs like warfarin or insulin, being off by even an hour can throw off your whole treatment. The CDC says 28% of seniors skip or delay doses because they’re confused about timing.Set phone alarms. Use a pill organizer with morning, afternoon, evening, and night compartments. If you take more than five medications, ask your pharmacist about a blister pack system-many pharmacies offer this for free. And remember: “as needed” doesn’t mean “whenever I feel like it.” If your doctor says take it only when your pain hits a 7/10, don’t take it at 3/10 just because you’re bored.
Rule 3: Don’t Mix Without Checking
You might think your multivitamin is harmless. But vitamin K can make blood thinners like warfarin useless. St. John’s Wort can cancel out antidepressants. Even grapefruit juice can turn a common cholesterol drug into a dangerous overdose. The FDA now requires warning labels on over 200 medications for food and supplement interactions.Before you add anything-herbal teas, OTC painkillers, supplements-ask your pharmacist or doctor. Bring all your bottles to your next appointment. This is called a “brown bag review.” Most clinics now offer it. It takes 15 minutes. It could save your life.
Rule 4: Understand Why You’re Taking It
Too many people just swallow pills because they were told to. But if you don’t know why, you won’t notice when something’s wrong. For example, if you’re on lisinopril for high blood pressure, you should know it might make you dizzy or cause a dry cough. If you’re on metformin, you should know it can cause stomach upset-and that’s normal at first.Ask your doctor: “What is this medicine supposed to do?” and “What side effects should I watch for?” If they say, “It’s just to lower your numbers,” push back. That’s not enough. You need to know how it helps you feel better-or prevent something worse. If you can’t explain your own medication to someone else, you don’t understand it yet.
Rule 5: Always Double-Check Before You Swallow
This is the most overlooked rule. Stop. Look. Read. Pause. Before you put any pill in your mouth, do a quick mental checklist:- Is this the right name? (Check the bottle)
- Is this the right dose? (Is it 5 mg or 50 mg?)
- Is this the right time? (Morning? After food?)
- Is this the right person? (If you’re helping someone else, confirm it’s their name on the label)
Studies show that simply pausing for 5 seconds before taking a pill reduces errors by 37%. That’s not magic. That’s human behavior. We rush. We multitask. We take pills while scrolling through our phones. Don’t. Make it a ritual. Sit down. Take a breath. Read the label out loud. It sounds silly-but it works.
What About Technology?
There are apps, smart pill dispensers, and barcode scanners in hospitals. But you don’t need fancy tech to stay safe. Still, if you use a smartphone, try a free medication tracker like Medisafe or MyTherapy. They send reminders, track refills, and even alert you if a new prescription might interact with something you’re already taking.And if you’re on Medicare or have a pharmacy benefit, ask if your insurer offers free medication therapy management. Pharmacists will call you quarterly to review all your meds-no appointment needed. In 2023, patients who used this service had 44% fewer emergency visits related to medications.

When Something Feels Off
Don’t ignore weird symptoms. New rash? Unexplained fatigue? Confusion? Diarrhea that won’t quit? These could be signs of a bad interaction, wrong dose, or allergic reaction. Don’t wait until your next checkup. Call your doctor or pharmacist right away. Keep a notebook. Write down what you took, when, and what happened. That’s the best tool you have.And if you ever feel pressured to take something “just in case,” or if a provider says, “It’s fine, trust me,” that’s a red flag. You have the right to ask questions. You have the right to say no. Your health isn’t a suggestion.
Final Thought: Safety Is a Habit, Not a One-Time Fix
Medication safety isn’t about being perfect. It’s about being consistent. One mistake won’t kill you. But repeating small errors over months or years? That’s how things go wrong. Make these five rules part of your daily routine. Write them on a sticky note. Put them on your bathroom mirror. Share them with a family member who helps you manage your meds.You’re not just taking pills. You’re managing your health. And that deserves your full attention.
What should I do if I miss a dose of my medication?
Don’t double up unless your doctor or pharmacist tells you to. For most medications, if you miss a dose by less than a few hours, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one and go back to your regular schedule. For blood thinners, insulin, or seizure meds, always check specific instructions-missing a dose can be dangerous. Keep a log so you can show your provider what happened.
Can I crush or split my pills?
Only if the label says it’s okay. Many pills-especially extended-release, enteric-coated, or capsule forms-are designed to release slowly. Crushing them can cause a dangerous overdose. If swallowing is hard, ask your doctor for a liquid version or a different form. Never split pills without a pill splitter and your pharmacist’s approval. Some pills have coatings that make splitting unsafe.
How do I know if my medication has expired?
Check the expiration date on the bottle or box. Most pills are safe for 1-2 years past that date if stored properly, but some-like insulin, liquid antibiotics, or nitroglycerin-lose effectiveness fast. If the pill looks discolored, cracked, or smells odd, throw it out. Don’t risk it. Many pharmacies offer free disposal bins for expired meds. Never flush them down the toilet unless the label says it’s safe.
Why do I need to tell my doctor about supplements I take?
Because supplements aren’t regulated like prescription drugs. A popular herb like turmeric can thin your blood, just like aspirin. Garlic supplements can interfere with HIV meds. Even vitamin C can affect how some chemotherapy drugs work. Your doctor needs the full picture to avoid dangerous interactions. Always list everything-even “natural” or “over-the-counter” products.
What should I do if I think I had a bad reaction?
Stop taking the medication immediately. Call your doctor or pharmacist. If you have trouble breathing, swelling of the face or throat, chest pain, or sudden confusion, call emergency services. Don’t wait. Write down what you took, when, and what symptoms you felt. Report the reaction to the FDA’s MedWatch program. Your report helps others avoid the same mistake.
Is it safe to take leftover antibiotics from a previous illness?
No. Antibiotics are prescribed for specific infections and specific bacteria. Taking leftover ones can lead to antibiotic resistance, make your infection worse, or cause side effects you didn’t have before. Even if you feel the same symptoms, it’s not the same illness. Always get a new prescription. Never share antibiotics with others.
Next Steps to Stay Safe
Start today. Pick one rule and make it a habit. Maybe it’s writing down your meds. Or setting a daily alarm. Or asking your pharmacist to explain one drug you’ve been taking for years. Small changes add up. In Perth, many pharmacies offer free medication reviews-just walk in with your bottles. No appointment needed. And if you’re caring for an older relative, sit down with them once a month and go through their pills together. You might catch something they missed.Medication safety isn’t about fear. It’s about control. You don’t have to be a doctor to protect yourself. You just have to pay attention.


Nosipho Mbambo 19.11.2025
Okay, but like… who actually does this? I mean, I forget if I took my pill or not ALL THE TIME. I just stare at the bottle like it’s gonna tell me. And then I take it anyway. 🤷♀️
Katie Magnus 19.11.2025
Ugh. Another ‘just read the label’ lecture. Like I don’t know how to take medicine. My grandma died because she trusted ‘the system.’ Now I don’t trust ANYTHING. Even my own prescriptions. 😭
King Over 19.11.2025
Rule 5 is the only one that matters. I do the pause thing. Just stop. Look. Breathe. Works every time. No apps needed. Just don’t be a zombie.
Johannah Lavin 19.11.2025
THIS. THIS. THIS. 💙 I’m a caregiver for my mom and we do the brown bag review every month. She used to hide her supplements ‘cause she didn’t want to be ‘a burden.’ Now she brings them out like a treasure chest. We laugh. We cry. We save lives. 🌸
Ravinder Singh 19.11.2025
Love this list - simple, practical, and human. I work in a pharmacy in Delhi and see the same mistakes daily. People take blood pressure meds with tea, crush pills because ‘it’s easier,’ and think ‘natural’ means ‘safe.’ I always say: if it’s medicine, it’s chemistry. Even turmeric. 🙏
My tip? Write the purpose on the bottle with a marker. ‘For blood pressure.’ ‘For nerves.’ ‘Don’t mix with alcohol.’ Makes it stick. Also, use a free app like Medisafe - it’s like having a nurse in your pocket. No ads, no spam. Just reminders.
And if you’re over 65? Ask your pharmacy about MTM - Medication Therapy Management. Free. No appointment. They’ll call you. Seriously. Do it.
Russ Bergeman 19.11.2025
1.3 million ER visits? That’s 0.4% of the population. So… 99.6% are fine? Maybe the problem isn’t the rules - it’s the people who can’t follow them. Also, ‘Tall Man lettering’? That’s a hospital thing. I’m not in a hospital. I’m in my kitchen. Stop overcomplicating.
Dana Oralkhan 19.11.2025
To the person who said ‘99.6% are fine’ - that’s not how safety works. One mistake can kill someone you love. I lost my brother to a mix-up with metformin and metoprolol. He didn’t know the difference. The pharmacist didn’t catch it. The doctor didn’t explain it. It wasn’t negligence. It was just… silence.
This post isn’t about fear. It’s about speaking up. Asking. Writing it down. Pausing. If you’re reading this, you’re already doing better than most. Keep going.
Jeremy Samuel 19.11.2025
nah bro. i just crush em and mix em in my coffee. works great. also i take my insulin with grapefruit juice. it’s like a morning shot. 🍊💉