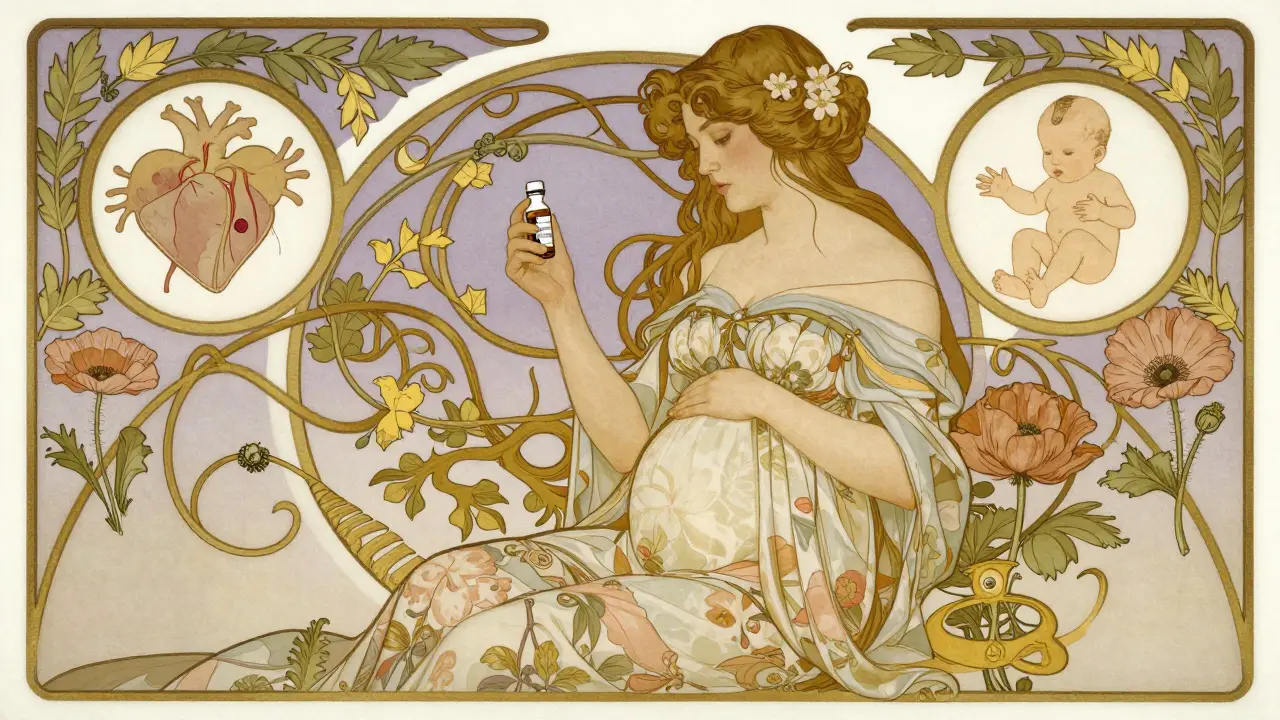
When a woman is pregnant and struggling with chronic pain, anxiety, or seizures, the question isn’t just gabapentin pregnancy safety-it’s whether the relief she needs is worth the potential cost to her baby. Gabapentin and pregabalin, known collectively as gabapentinoids, are widely prescribed for conditions like neuropathic pain, fibromyalgia, and epilepsy. But as their use in pregnant women has surged-rising from 0.2% of pregnancies in 2000 to nearly 4.2% today-the evidence about their effects on fetal development has become harder to ignore.
What Do We Know About Birth Defects?
The biggest fear for any expectant parent is a major birth defect. The most comprehensive study to date, published in PLOS Medicine in 2020, tracked over 1.7 million pregnancies and found that gabapentin use during the first trimester did not significantly raise the overall risk of major congenital malformations. The relative risk was just 1.07-meaning a tiny increase from a baseline of about 3% to 3.21%. That’s far lower than drugs like valproic acid, which can push malformation risk above 10%. But here’s the catch: not all risks are equal. The same study found a clear signal for specific heart defects, especially conotruncal abnormalities like tetralogy of Fallot. The risk doubled (RR=1.40) when gabapentin was taken consistently-two or more prescriptions-during early pregnancy. That translates to an absolute risk increase from 0.59% to 0.82%. It’s rare, but it’s real. And unlike other antiseizure medications, this cardiac signal wasn’t seen with lamotrigine, a safer alternative for many. Pregabalin, while less studied in humans, has raised red flags in animal research. The European Medicines Agency flagged developmental toxicity in lab animals, and its label now warns against use in pregnancy unless benefits clearly outweigh risks. In practice, many doctors are shifting away from pregabalin in favor of gabapentin when medication is unavoidable.Neonatal Adaptation: A Hidden Risk
Most people focus on birth defects. But the real challenge often comes after birth. Babies exposed to gabapentinoids late in pregnancy-especially if the mother took it regularly until delivery-show signs of neonatal adaptation syndrome. Think jitteriness, irritability, feeding problems, tremors, and even breathing difficulties. One study found that 38% of infants exposed to gabapentin until delivery needed NICU admission, compared to just 2.9% of unexposed babies. This isn’t opioid withdrawal, but it’s similar in presentation. The drug crosses the placenta easily. With a half-life of 5-7 hours and standard doses of 300-3600 mg per day, the fetus is constantly exposed. When the baby is born and that supply stops, their nervous system struggles to adjust. The risk isn’t just about dose-it’s about timing. Taking gabapentin in the third trimester carries the highest risk for these issues.Preterm Birth and Growth Issues
The data doesn’t stop at the newborn period. Studies show that women taking gabapentin during pregnancy are more likely to deliver early. The relative risk for preterm birth is 1.34. That means about 34% more preterm deliveries than in unexposed pregnancies. And babies are more likely to be small for gestational age-1.22 times more likely, according to the same large-scale analysis. These aren’t minor concerns. Preterm birth is the leading cause of newborn complications worldwide. Babies born early face higher risks of breathing problems, brain bleeds, infections, and long-term developmental delays. Even if a baby doesn’t have a major defect, being born too early or too small can change their entire trajectory.
How Does Gabapentin Affect the Developing Brain?
Beyond structure and immediate outcomes, there’s growing concern about how gabapentin impacts brain development at the cellular level. A 2022 study from China exposed developing nerve cells to therapeutic levels of gabapentin-and saw dramatic changes. Dopaminergic neurons, which are critical for movement, mood, and reward pathways, showed a 37-42% reduction in nerve growth. Key genes like Nurr1, En1, and Bdnf, which guide brain development, were significantly downregulated. These aren’t theoretical findings. They’re lab results from human-derived neurons. And they suggest that even if a baby looks fine at birth, there could be subtle, long-term effects on brain wiring. That’s why the NIH has launched a major study tracking 1,200 children exposed to gabapentin in utero until age five. Results are expected in late 2025. Until then, we’re operating with incomplete data.What Do Experts Recommend?
Guidelines are shifting. The American College of Obstetricians and Gynecologists (ACOG) says gabapentin should only be used if non-drug options have failed and the condition is severe enough to justify the risk. The British National Formulary says to avoid it unless benefits clearly outweigh toxicity. The FDA still labels both drugs as Category C-meaning risk can’t be ruled out, but benefits might justify use. Many clinicians are now treating gabapentin like a last resort. For someone with severe neuropathic pain that’s unresponsive to physical therapy, acupuncture, or non-opioid pain relievers, gabapentin may be the only option that works. But for anxiety, insomnia, or mild chronic pain? There are safer alternatives. Duloxetine is now preferred in many cases. Non-pharmacological therapies like cognitive behavioral therapy (CBT) and mindfulness-based stress reduction have strong evidence for pain and anxiety management during pregnancy.What Should You Do If You’re Taking Gabapentin and Pregnant?
If you’re already taking gabapentin and find out you’re pregnant, don’t stop cold turkey. Sudden withdrawal can trigger seizures or rebound pain. Talk to your doctor immediately. Together, you can weigh:- Why you’re taking it (pain? epilepsy? anxiety?)
- How long you’ve been on it
- What dose you’re on
- When you’re in your pregnancy
- Whether safer alternatives exist

What About Breastfeeding?
Gabapentin does pass into breast milk, but in low amounts. The AAP considers it compatible with breastfeeding, and most studies show no adverse effects in nursing infants. Pregabalin is less studied, but appears to transfer in similar low levels. Still, watch your baby closely for drowsiness, poor feeding, or unusual fussiness. If your baby seems unusually sleepy or isn’t gaining weight well, talk to your pediatrician.What’s Changing Now?
The FDA just required all gabapentinoid manufacturers to conduct post-marketing surveillance of 5,000 pregnancy outcomes by 2027. That’s a big step. Right now, most safety data comes from observational studies-useful, but not perfect. A formal, long-term registry will give us clearer answers. Meanwhile, pregabalin use in pregnancy is expected to drop 25-35% by 2027. Doctors are moving toward alternatives, and insurers are starting to restrict coverage for pregabalin in pregnant patients. Non-drug therapies are gaining more insurance support too.Bottom Line: Risk Is Real, But Not Absolute
Gabapentin isn’t a dangerous drug for every pregnant woman. But it’s not harmless either. The risk of major birth defects is low. The risk of preterm birth, growth issues, and neonatal withdrawal is higher-and often overlooked. The cardiac risk is small but real. The long-term brain effects? Still unknown. If you need it-for severe, unmanageable pain, for example-it may still be the best option. But if you’re taking it for mild pain, anxiety, or sleep? There are safer paths. Don’t assume it’s fine because your doctor prescribed it. Ask: Is there a better alternative? What’s the evidence? What are we watching for? This isn’t about fear. It’s about informed choice. And the data is finally catching up to the reality of how widely these drugs are used during pregnancy.Is gabapentin safe during pregnancy?
Gabapentin is not considered completely safe during pregnancy. While it doesn’t significantly increase the overall risk of major birth defects, it’s linked to a higher chance of preterm birth, babies being small for gestational age, and neonatal withdrawal symptoms like irritability and feeding problems. There’s also a small but real increased risk of specific heart defects when taken consistently in early pregnancy. It should only be used if other treatments have failed and the benefit clearly outweighs the risk.
Can gabapentin cause birth defects?
Gabapentin doesn’t cause a broad increase in birth defects, but it is associated with a slightly higher risk of specific heart defects, particularly conotruncal abnormalities like tetralogy of Fallot. The absolute risk goes from about 0.59% in unexposed pregnancies to 0.82% in those exposed to gabapentin consistently during the first trimester. This risk is much lower than drugs like valproic acid but higher than safer alternatives like lamotrigine.
What are the risks of taking gabapentin in the third trimester?
Taking gabapentin in the third trimester carries the highest risk for neonatal adaptation syndrome. Babies may be born jittery, irritable, have trouble feeding, or need NICU care. About 38% of infants exposed until delivery required NICU admission, compared to just 2.9% of unexposed babies. It also increases the risk of preterm birth and low birth weight. Stopping gabapentin suddenly isn’t safe either-always work with your doctor to taper if needed.
Is pregabalin safer than gabapentin in pregnancy?
No, pregabalin is not considered safer. Animal studies show developmental toxicity, and regulatory agencies like the EMA advise against its use in pregnancy unless absolutely necessary. While human data is more limited, experts are moving away from pregabalin in pregnant patients due to stronger safety signals. Gabapentin is currently the preferred option if medication is unavoidable, but both carry risks.
Can I breastfeed while taking gabapentin?
Yes, gabapentin is generally considered compatible with breastfeeding. It passes into breast milk in low amounts, and most studies haven’t found harmful effects in nursing infants. However, monitor your baby for unusual drowsiness, poor feeding, or fussiness. If you notice any changes, talk to your pediatrician. Pregabalin is less studied, but appears to transfer in similar low levels.
What are safer alternatives to gabapentin during pregnancy?
For neuropathic pain, duloxetine is often preferred over gabapentin. For anxiety or depression, cognitive behavioral therapy (CBT) and mindfulness have strong evidence and no fetal risk. Physical therapy, acupuncture, and non-opioid pain relievers like acetaminophen (used cautiously) may help. For epilepsy, lamotrigine is considered one of the safest antiseizure medications during pregnancy. Always discuss alternatives with your doctor before making changes.

Nancy Kou 19.12.2025
This is one of the most balanced, data-driven pieces I’ve read on gabapentin in pregnancy. Finally, someone broke down the real risks without fearmongering or downplaying the neonatal adaptation syndrome. The 38% NICU rate for late-trimester exposure? That’s the number that needs to be shouted from the rooftops. Doctors keep saying 'it's just a mild withdrawal' like it's a bad night's sleep. It’s not. It’s a newborn screaming because their nervous system got yanked off a drug train.
Connie Zehner 19.12.2025
OMG I’m so glad someone finally said this!! I took gabapentin for anxiety during both pregnancies and my kids are perfectly fine!! One’s in Harvard, the other’s a pro soccer player!! So stop scaring people!! It’s not a drug, it’s a miracle!! 🙏
holly Sinclair 19.12.2025
What’s fascinating to me is how we treat gabapentin as this benign, almost herbal supplement when it’s clearly a neuroactive compound that crosses the placenta with ease. We don’t give SSRIs to pregnant women without weighing neurodevelopmental trade-offs, yet gabapentin gets a free pass because it’s not an 'antidepressant.' But if it’s altering dopaminergic neuron growth in human-derived cells by 40%, then it’s not just a 'mild' drug-it’s a developmental modulator. The NIH’s 5-year study is the bare minimum. We need longitudinal neuroimaging of these kids. We’re playing Russian roulette with neural wiring and calling it 'informed consent.'
Hussien SLeiman 19.12.2025
Oh here we go again. The 'gabapentin is dangerous' crowd. Let’s not forget that 99% of babies exposed to it are born without major defects. You’re acting like every woman who takes it is a reckless monster. Meanwhile, women with chronic neuropathic pain are being told to 'just endure it' like it’s a bad backache. What’s more unethical? Prescribing a drug with a 0.8% increased risk of a rare heart defect, or forcing a woman into uncontrolled seizures because you’re afraid of a few extra NICU days? The real villain here is the medical system that offers no alternatives and then blames the patient for needing help.
Tim Goodfellow 19.12.2025
Man, I’ve seen this play out in the ER-newborns trembling like they’ve got the shakes, moms crying because they didn’t know gabapentin could do this. One lady told me she thought it was 'like Advil for nerves.' We’re not talking about a vitamin. We’re talking about a molecule that rewires developing synapses. And now the FDA’s finally waking up? Took ‘em long enough. I’ve been begging for a registry since 2020. The fact that pregabalin’s use is dropping 30% by 2027? That’s the first good news in years. Let’s hope insurers follow suit and fund CBT like they fund prescriptions.
Elaine Douglass 19.12.2025
I’m 28 weeks and on gabapentin for fibro pain. I read this and cried. I didn’t know about the NICU stats. My doctor just said 'it’s fine.' I’m going to ask about duloxetine tomorrow. Thank you for writing this. I feel less alone.
Lynsey Tyson 19.12.2025
Just wanted to say thank you to everyone sharing their stories here. This is the kind of conversation we need more of-not fear, not judgment, just real info from real people. I’m so glad we’re finally talking about the neonatal stuff. I didn’t know about the brain development stuff either. Feels like we’ve been kept in the dark for too long. Let’s keep this going.
Kelly Mulder 19.12.2025
It is a matter of profound moral irresponsibility that pharmaceutical entities continue to market gabapentinoids as 'low-risk' for gestational populations while the preclinical and epidemiological data demonstrate a statistically significant association with neurodevelopmental perturbations. The FDA’s Category C designation is a euphemism for 'we have no idea.' The onus is now on clinicians to eschew convenience and prioritize evidence-based alternatives. Duloxetine, CBT, acupuncture-these are not 'alternatives.' They are the standard of care. To prescribe gabapentin for insomnia or mild anxiety during pregnancy is not medical practice. It is negligence dressed in white coats.
Isabel Rábago 19.12.2025
So if I took gabapentin for anxiety in my first trimester and my kid is now 3 and hitting all milestones, does that mean it’s safe? Or am I just lucky?