Every year, over 2.1 million people in the U.S. call the Poison Control Hotline for help with accidental or intentional poisonings - and nearly half of those calls are about medications. Whether it’s a child who grabbed a bottle of pills, an adult who took the wrong dose, or someone unsure if a mix of drugs is dangerous, this free service can prevent hospital visits, serious injury, or even death. But most people don’t know what to say when they call - or if they even should.
How the Poison Control Hotline Actually Works
The Poison Control Hotline isn’t just a phone number. It’s a nationwide network of 53 accredited centers staffed by Specialists in Poison Information (SPIs), most of whom are pharmacists, nurses, or doctors with advanced training in toxicology. You can reach them by dialing 1-800-222-1222, texting "poison" to 797979, or using the webPOISONCONTROL tool at poisonhelp.org. No matter how you contact them, your call is routed to the center nearest you based on your area code.These specialists don’t guess. They use over 1,500 evidence-based algorithms developed by toxicology experts to assess risk. Each algorithm is built on real-world data from millions of past cases. When you call about a medication, they don’t ask for your name, insurance, or address. They ask for facts: what you took, how much, when, and how the person is feeling. That’s it.
The system is fast. The average call lasts 8 to 12 minutes. About 60% of medication-related cases are handled at home - no ambulance, no ER. That’s because poison control centers have one goal: keep you safe without unnecessary medical intervention. A 2019 study found this system saves the U.S. healthcare system nearly $1.8 billion a year by avoiding preventable hospital visits.
What You Must Report About Medications
If you’re calling because of a medication issue, the more precise you are, the better the advice you’ll get. Vague answers lead to vague or wrong guidance. Here’s exactly what they need:- Exact medication name - not just "Tylenol," but "Tylenol Extra Strength, 500mg per tablet." If it’s a generic, say "acetaminophen 500mg." Brand and generic names matter because some products look alike but contain different doses.
- Amount ingested - "three pills" isn’t enough. Say "three 500mg tablets" or "15 mL of liquid cough syrup." If you’re not sure, bring the bottle to the phone.
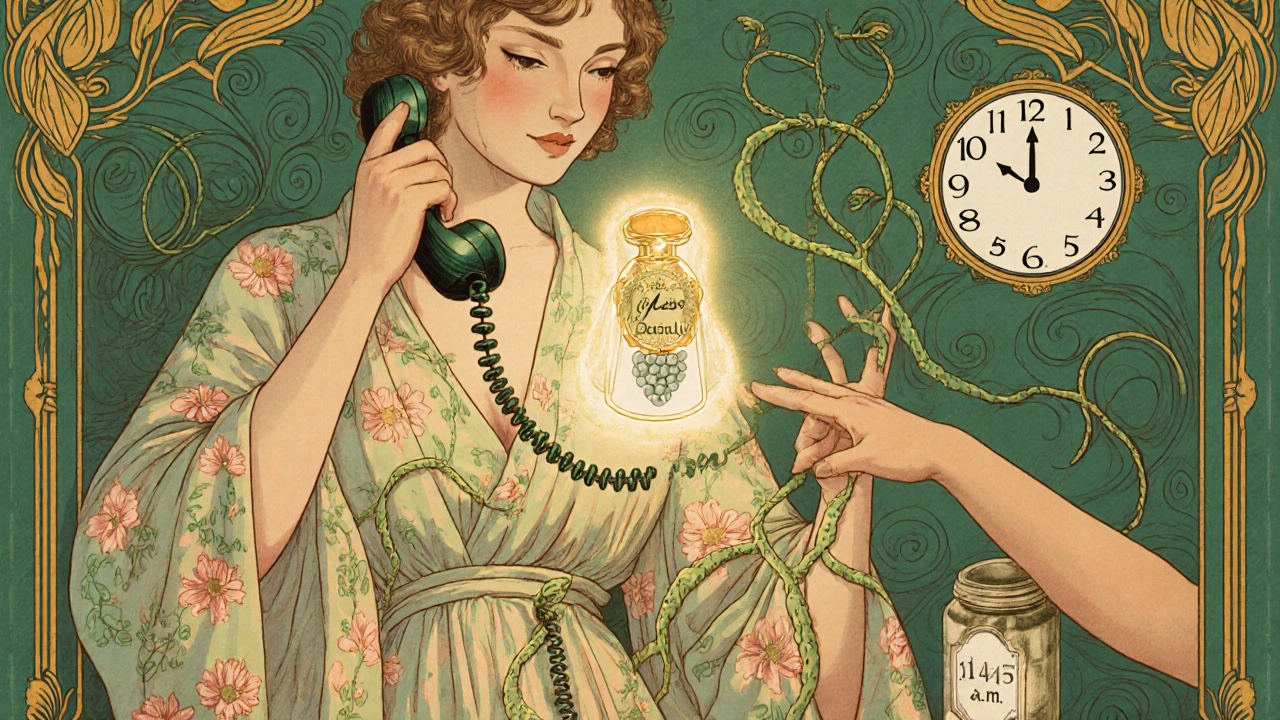
- Time of exposure - "an hour ago" is too vague. Say "10:45 a.m." or "about 45 minutes ago." Timing affects treatment, especially with drugs like acetaminophen or opioids.
- Patient’s age and weight - weight in kilograms is best. If you don’t know it, estimate. A 20-pound child is not the same as a 180-pound adult. Dose calculations depend on this.
- Any symptoms - drowsiness? vomiting? confusion? blurred vision? Even small changes matter. Don’t wait for "serious" signs. Call at the first hint of trouble.
Here’s a real example: A parent calls because their 3-year-old swallowed half a bottle of melatonin gummies. They say, "I think she ate 10 gummies." The specialist asks: "What’s the strength per gummy?" "10 mg." "When?" "About 20 minutes ago." "Is she sleepy?" "Yes, and she’s drooling." Within minutes, the specialist says: "Keep her awake, give her water, watch for breathing changes. Call back if she becomes unresponsive." No ER needed. No sedation. Just smart, fast advice.
Why Polypharmacy Is a Big Red Flag
One of the most dangerous situations poison control sees is when someone takes multiple medications together. About 32% of serious medication poisonings involve drug interactions. It’s not just about one pill being too much - it’s about how they react with each other.For example, mixing a prescription opioid with a sleep aid or an anti-anxiety drug can slow breathing to dangerous levels. Taking blood pressure meds with certain herbal supplements can drop your blood pressure too far. Even over-the-counter painkillers like ibuprofen can interact with blood thinners or kidney medications.
When you call, list every medication - including vitamins, supplements, and creams. Don’t leave anything out. The specialists have databases that flag interactions you didn’t even know existed. They’ve seen cases where people thought they were safe because each drug was prescribed separately - until they were taken together.

What Happens After You Call
You might think the call ends when the specialist gives you instructions. But often, it’s just the beginning. For high-risk exposures - like acetaminophen, opioids, or antidepressants - poison control will schedule follow-up calls. For acetaminophen, they’ll call back at 4, 8, and 24 hours to check liver enzyme levels and symptoms. They’ve tracked over 90% of these follow-ups successfully.You’ll also get an email summary with everything discussed: exact product names, risk level, instructions, and when to call back. Most people save this email. It’s helpful when talking to a doctor later or if symptoms worsen.
Some calls lead to hospital transport. That’s not a failure - it’s a success. The goal isn’t to avoid hospitals at all costs. It’s to make sure you go to the right place at the right time. Poison control specialists know which cases need emergency care and which can be managed safely at home.
What They Can’t Help With
The Poison Control Hotline is powerful, but it’s not magic. There are limits:- They don’t handle intentional overdoses if you’re calling for someone else - if someone is unconscious or not breathing, call 911 first.
- They can’t help if more than two substances were involved. That’s too complex for the algorithm. You’ll need to speak with a specialist directly.
- They don’t replace emergency care. If someone is having seizures, stopping breathing, or is unconscious, dial 911 immediately. Then call poison control while help is on the way.
Also, the webPOISONCONTROL tool doesn’t work for intentional overdoses or complex cases. It’s designed for accidental exposures. If you’re unsure, always call the phone line. Humans are better at handling uncertainty.
Who Uses It and Why
The most common callers are parents. Nearly half of all medication poisonings involve children under 6. But adults use it too - especially older adults managing multiple prescriptions, or people who accidentally take a double dose.One Reddit user, a pharmacist, shared how poison control helped prevent liver failure in a child who swallowed 12 acetaminophen tablets. The specialist instructed the parent to give N-acetylcysteine within the 8-hour window - the critical time for reversing toxicity. The child recovered fully. No hospital stay. No long-term damage.
Surveys show 94.7% of users rate the advice as "excellent" or "good." People especially appreciate how specialists understand brand-name and generic equivalents, even across international products. If you’re visiting from Canada or Europe and your meds have different names, they’ll still know what you mean.

How It’s Funded and Why It’s Free
You don’t pay for poison control. Ever. It’s funded by government grants (62%), hospital support (28%), and state funding (10%). Total annual budget: about $125 million. That’s less than the cost of one new MRI machine in a single hospital.For every dollar spent on poison control, society gains $7.67 in saved medical costs and lost productivity. That’s why the American Medical Association calls it essential public health infrastructure. Hospitals all over the country have formal agreements with their local poison center. ER doctors call them before giving treatments. They trust the data.
What’s Changing Now
The threats are evolving. From 2018 to 2022, medication poisonings rose 18.7%. Opioids went up 22.3%. Sedatives, 19.8%. Weight-loss drugs like semaglutide (Ozempic) are now showing up in poison control reports with unexpected side effects.New tools are coming. The National Poison Data System (NPDS) now shares data with 42 major hospital networks. That means if you go to the ER after calling poison control, the doctor already has your case history. AI is being trained to recognize new synthetic drugs faster. And 31 centers now offer video consults for complex cases.
But funding is under pressure. Inflation could cut service capacity by 12-15% without more money. That’s why every call matters - not just for you, but for keeping the system alive.
Bottom Line: Call Early, Call Often
Don’t wait to see if symptoms get worse. Don’t Google it. Don’t assume it’s "probably fine." If you’re even a little worried about a medication - whether it’s a child, an elderly parent, or yourself - call 1-800-222-1222. It’s free. It’s fast. It’s backed by decades of science.You don’t need to be an expert. You don’t need to know the name of the drug perfectly. Just have the bottle nearby. Say what you know. The specialists will ask the rest.
And if you ever forget the number, save it in your phone right now. Put it next to your emergency contacts. Because when it matters, you won’t want to be searching.
When should I call the Poison Control Hotline for a medication issue?
Call immediately if someone has taken more than the recommended dose, if a child has accessed medication, if you’re unsure about a drug interaction, or if any symptoms appear - even mild ones like drowsiness, nausea, or dizziness. Don’t wait for severe symptoms. Early calls lead to better outcomes.
Do I need to give my name or insurance info when I call?
No. Poison Control is completely confidential. You don’t need to give your name, address, or insurance details. They only need the medication name, amount, time, patient age/weight, and symptoms. Your privacy is protected under HIPAA.
Can I use the webPOISONCONTROL app instead of calling?
Yes, for most accidental exposures involving one or two medications. The app guides you through six key questions and gives instant advice. But if the person is unconscious, having trouble breathing, or took more than two substances, call 1-800-222-1222 instead. The app doesn’t handle emergencies or complex cases.
Is the Poison Control Hotline available 24/7?
Yes. The Poison Control Hotline (1-800-222-1222) operates 24 hours a day, 7 days a week, 365 days a year. There is never a time when you can’t reach a specialist. Texting "poison" to 797979 also works around the clock.
What if I’m not sure what the medication is?
Bring the bottle to the phone. Even if the label is faded, the shape, color, and imprint code (like "AP 500") can help specialists identify it. If you can’t find the bottle, describe it: color, shape, size, any markings. The more detail, the better the chance of correct identification.
Does poison control help with herbal supplements and vitamins?
Yes. Many people assume supplements are safe, but high doses of vitamins (like vitamin D or iron), herbal products (like kava or comfrey), or weight-loss supplements can be toxic. Poison control tracks over 1,000 supplement-related exposures annually. Always report them when calling.
How accurate is the webPOISONCONTROL tool?
Studies show the webPOISONCONTROL tool matches human specialist recommendations 97.3% of the time. It’s been used in over 1.2 million cases since 2014. But it’s designed for single-substance, accidental exposures. For complex cases, always call the hotline.
Are poison control services available in languages other than English?
Yes. The hotline provides translation services in over 150 languages. Just say the language you need, and a translator will join the call. This includes Spanish, Mandarin, Arabic, Vietnamese, and many Indigenous languages. No one is turned away for language barriers.

james lucas 22.11.2025
man i had no idea this service was this legit 😅 i thought it was like one of those automated bots that say "call 911" but nooo they actually have pharmacists on the line?? my aunt took 3 extra strength tylenol by accident last year and called them outta panic and they told her to drink water and watch for nausea for 4 hours and she was fine. no hospital. no bill. just chill advice. why isn’t this on every phone like 911??
Jessica Correa 22.11.2025
so many people think supplements are harmless but like i had a friend take 10 iron pills because she thought it would "boost energy" and ended up in the er and poison control was the one who told the doctors exactly what to do because she had the bottle with her and they knew the dosage and timing. they’re unsung heroes
manish chaturvedi 22.11.2025
In India, we often underestimate the danger of over-the-counter medications. Many people consume multiple painkillers simultaneously without understanding interactions. The Poison Control Hotline model described here is not only efficient but also culturally scalable. In countries with limited healthcare infrastructure, such systems can be life-saving. I encourage global health organizations to adopt similar frameworks, especially in regions where pharmacy access is inconsistent.
Nikhil Chaurasia 22.11.2025
i just… i can’t believe how much i took for granted. my dad took his blood pressure med and then a cold med with decongestant and passed out on the couch. we called 911 but they told us to call poison control too. the lady on the line asked three questions and said "he’s gonna be fine but keep him awake" and she was right. she didn’t even ask my name. just what he took and when. i cried after hanging up. that’s not tech. that’s humanity.
Holly Schumacher 22.11.2025
Let me just say this: the fact that you’re still using the term "melatonin gummies" as if they’re harmless candy is a national tragedy. These are not gummy bears. They’re sedative payloads with sugar coatings. And yes, I’ve seen the ER reports. A 5-year-old ingesting 20 mg of melatonin is not "a little sleepy," it’s a chemical assault on a developing brain. The webPOISONCONTROL tool is 97% accurate? That’s not a feature - it’s a terrifyingly low bar. Someone should audit the algorithm for pediatric dosing thresholds. This isn’t a public service - it’s a band-aid on a hemorrhage.
Michael Fitzpatrick 22.11.2025
my grandma’s on like 12 different meds and i used to be scared to even ask her if she took her pills right. now i just keep the poison control number saved in my phone and we have a little ritual - every sunday we go through her pillbox together and if something looks weird we call them. they helped us figure out that her fish oil was interacting with her blood thinner and they told us to switch brands. no drama. no judgment. just clear advice. i wish every family had this safety net
Shawn Daughhetee 22.11.2025
just saved it to my contacts right now. i always thought "if i take too much ibuprofen i’ll just sleep it off" but now i know that’s dumb. i’m telling my whole family. my cousin’s kid just started taking ADHD meds and i’m gonna make sure they know this number
Miruna Alexandru 22.11.2025
The systemic underfunding of poison control centers is a microcosm of how we commodify health outcomes. We optimize for cost avoidance rather than preventive infrastructure. The $7.67 return on investment is not a success metric - it’s a moral indictment. Why do we fund military drones over poison control? Why do we treat toxicity as an individual failure rather than a public health design flaw? The algorithmic triage works - but only because we’ve normalized the expectation that people will be poisoned in the first place.
Justin Daniel 22.11.2025
so i called them once because i thought i ate a mushroom that looked like a button mushroom but was actually a death cap. they didn’t laugh. they didn’t ask if i was high. they just said "describe the gills" and then told me to go to the ER and they called ahead for me. i still don’t know how they knew it was a death cap from my description but i’m alive so i’m not questioning it. also they sent me an email with a picture of the mushroom. that’s next level
Melvina Zelee 22.11.2025
you know what’s wild? the fact that poison control doesn’t ask for your insurance or name means they treat you like a human not a billing code. i used to think healthcare was about who you know or how much you pay but this? this is the only thing i’ve ever seen that actually works for everyone the same way. no matter if you’re rich or broke or new to the country or just forgot what your meds are called. they don’t care about your background. they care about your liver. that’s the kind of system i want to live in
Kezia Katherine Lewis 22.11.2025
It’s worth noting that the NPDS integration with hospital EHRs represents a paradigm shift in real-time toxicovigilance. The syndromic surveillance capability now allows for rapid identification of novel drug adulterants - particularly synthetic cannabinoids and fentanyl analogs - which previously evaded detection due to their structural variability. This is the future of clinical toxicology: predictive, networked, and data-driven.