Semaglutide isn’t just another weight loss drug. It’s reshaping how we treat obesity - not as a moral failing or lack of willpower, but as a biological condition with real, measurable effects on the brain and body. If you’ve heard about Ozempic or Wegovy in the news, on social media, or from a friend, you’re not alone. Millions are using it. But what does it actually do? And why do some people lose 20% of their body weight while others stop after a few months?
What Semaglutide Actually Does in Your Body
Semaglutide mimics a natural hormone called GLP-1 - glucagon-like peptide-1 - that your gut releases after eating. This hormone tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin only when needed. But unlike the natural version, which lasts minutes, semaglutide sticks around for days. That’s because it binds to albumin in your blood, protecting it from being broken down too quickly. This is why you only need one injection per week.
Here’s the science behind the weight loss: semaglutide targets specific neurons in your hypothalamus - the part of your brain that controls hunger. It turns down the volume on hunger signals (NPY and AgRP neurons) and turns up the volume on fullness signals (POMC and CART neurons). Think of it like rewiring your appetite dial from ‘starving’ to ‘satisfied’ without needing to eat more. It doesn’t just suppress appetite - it changes how food tastes and smells to you. Many users report that fatty or sugary foods suddenly feel overwhelming, even unappealing.
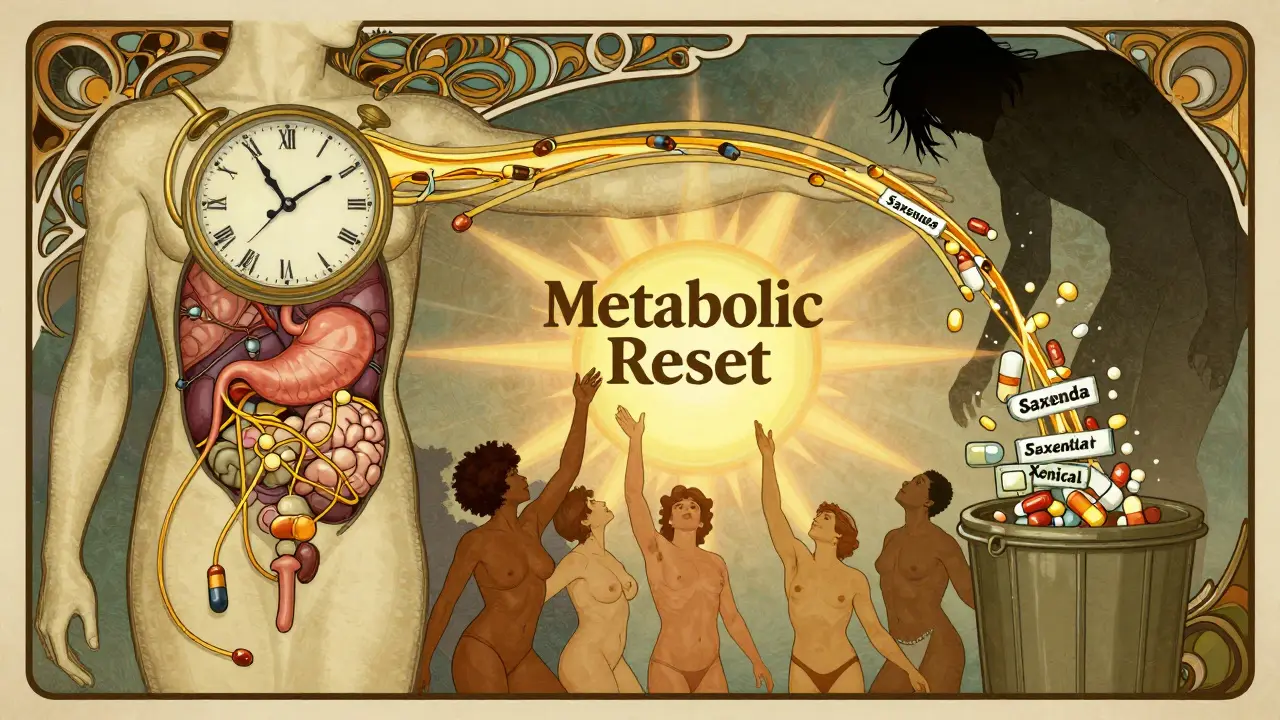
It also works on your metabolism. Studies show semaglutide helps turn white fat - the kind that stores energy - into brown fat, which burns energy. It improves insulin sensitivity, reduces liver fat, and lowers inflammation. These aren’t side effects. They’re core mechanisms that make semaglutide more than an appetite suppressant. It’s a metabolic reset.
Ozempic vs. Wegovy: Same Drug, Different Doses
Ozempic and Wegovy are both semaglutide. The only difference is the dose and what they’re approved for.
- Ozempic: 0.5 mg or 1 mg weekly. Approved for type 2 diabetes. Many people use it off-label for weight loss.
- Wegovy: 2.4 mg weekly. Approved specifically for chronic weight management in adults with obesity or overweight plus a weight-related condition (like high blood pressure or sleep apnea).
It’s not that Ozempic doesn’t cause weight loss - it does. But Wegovy’s higher dose triggers stronger effects. In the STEP 1 trial, people on Wegovy lost an average of 14.9% of their body weight over 68 weeks. That’s about 33 pounds for someone weighing 220 pounds. Only 2.4% lost that much on placebo. The difference? More than 12 percentage points.
One key point: Wegovy was designed for weight loss. Ozempic was designed for blood sugar control. While both work, Wegovy’s dosing schedule and clinical data are built around maximizing weight loss, not just managing diabetes.
How Effective Is It? Real Numbers, Not Hype
Let’s cut through the noise. In the STEP 1 trial:
- 69-79% of people lost at least 10% of their body weight.
- 48-58% lost 15% or more.
- 32% lost 20% or more.
Compare that to older weight loss drugs like liraglutide (Saxenda), which helped people lose about 8% on average. Or orlistat (Xenical), which averaged 5%. Semaglutide isn’t just better - it’s in a different league.
But here’s the catch: it works best when paired with lifestyle changes. The STEP trials didn’t just give people injections. They gave them weekly counseling on nutrition and physical activity. The people who lost the most weight weren’t just on the drug - they were eating differently, moving more, and sleeping better. Semaglutide doesn’t replace healthy habits. It makes them easier to stick to.

The Downside: Side Effects and Real-Life Struggles
Almost everyone experiences some side effects - especially early on. In clinical trials:
- 77% had nausea
- 64% had diarrhea
- 56% had vomiting
That’s a lot. But most people get used to it. The trick is starting low and going slow. Wegovy’s dosing schedule isn’t random - it’s designed to reduce nausea. You begin at 0.25 mg per week for four weeks, then increase every four weeks until you hit 2.4 mg. Rushing this process increases the chance of quitting.
Some people can’t tolerate it at all. Reddit threads are full of stories like: “I couldn’t get past 1.7 mg. The nausea was constant.” Others report dizziness, fatigue, or constipation. These aren’t rare. They’re expected.
There’s also a rare but serious risk: thyroid tumors in rats. The FDA requires a warning because of this, though no clear link has been found in humans. It’s contraindicated if you or a close family member has had medullary thyroid cancer or Multiple Endocrine Neoplasia Syndrome Type 2.
What Happens When You Stop?
This is the part no one talks about enough. In the STEP 4 trial, people who stayed on semaglutide kept 10.6% of their weight off after 68 weeks. Those who switched to placebo? They regained 6.9% of their body weight - about two-thirds of what they lost.
That means: if you stop, you’ll likely gain most of it back. Not because you’re weak. Not because you “slipped up.” Your biology reverts. Your hunger signals return. Your metabolism slows. The drug was holding back a biological drive that never went away.
Dr. Fatima Cody Stanford put it bluntly: “This isn’t a cure. It’s a tool for lifelong management.” If you need semaglutide to stay at a healthy weight, you may need it indefinitely. That’s not failure. It’s like taking blood pressure medication - you don’t stop because you feel better. You keep taking it because the condition doesn’t disappear.
Cost, Access, and the Bigger Picture
Wegovy costs around $1,350 per month in the U.S. without insurance. That’s more than most people can afford. Even with insurance, many plans require prior authorization, step therapy, or don’t cover weight loss drugs at all. A 2023 American Medical Association survey found 78% of providers had patients unable to get their prescribed dose due to shortages.
On Trustpilot, Wegovy has a 2.1/5 rating - not because it doesn’t work, but because people can’t get it, can’t afford it, or can’t keep it. One user wrote: “I lost 50 pounds. Insurance dropped coverage after 6 months. I gained it all back in 10 weeks.”
Novo Nordisk offers a patient assistance program for eligible uninsured or underinsured people. But the system is broken. We have a drug that can transform lives - and millions can’t access it.
Who Is It For? And Who Should Avoid It?
Semaglutide works best for:
- Adults with obesity (BMI ≥30)
- Adults with overweight (BMI ≥27) and at least one weight-related condition (hypertension, prediabetes, sleep apnea, etc.)
- People who’ve tried diet and exercise but plateaued
- Those willing to accept side effects and commit to long-term use
It’s not for everyone. Avoid it if you:
- Have a personal or family history of medullary thyroid cancer
- Have Multiple Endocrine Neoplasia Syndrome Type 2
- Are pregnant or breastfeeding
- Have a history of pancreatitis (though evidence is mixed)
And it’s not a magic pill for people who just want to lose 10 pounds for a wedding. It’s for people with clinically significant obesity who need real, lasting help.
The Future: What’s Next After Semaglutide?
Semaglutide isn’t the end - it’s the beginning. Tirzepatide (Mounjaro, Zepbound), a dual GLP-1 and GIP agonist, has shown even better results: up to 20.9% weight loss in trials. Oral semaglutide (Rybelsus) is approved for diabetes and being tested for weight loss - if it works, it could be a game-changer for people who hate injections.
Researchers are also testing semaglutide in adolescents (ages 12-17), with early results showing promise. And combination therapies - like pairing semaglutide with other appetite regulators - could push weight loss beyond 25%.
But the biggest challenge isn’t science. It’s sustainability. Can we afford to give this to millions? Can our healthcare system handle lifelong prescriptions? Will insurance ever cover it like insulin or statins?
For now, semaglutide is the most powerful tool we have for obesity treatment. But it’s not a cure. It’s a bridge - one that works best when paired with support, education, and long-term care.


Paul Mason 6.01.2026
Semaglutide ain't magic, but it's the closest thing we got. I watched my mate drop 40 lbs on Wegovy - not because he was ‘disciplined,’ but because his brain finally stopped screaming for chips at 2am. The nausea? Yeah, it sucked for a bit. But once you dial in the dose, it’s like your body finally shuts up and listens.
Katrina Morris 6.01.2026
so i lost 35 lbs on ozempic but my insurance dropped me after 6 months and i gained it all back like a boomerang 😔 the system is so broken i just cry sometimes
LALITA KUDIYA 6.01.2026
in india we dont even have access to this unless you pay out of pocket and its like 5x the price 😞 but still amazing science! i hope it gets cheaper soon 🙏
Poppy Newman 6.01.2026
the fact that it makes junk food taste like cardboard?? 😍 i used to snack all day. now i look at a donut and think ‘nah, not worth it.’ weird, but life-changing 💫
Christine Joy Chicano 6.01.2026
It’s astonishing how the pharmaceutical industry has weaponized neurobiology to reframe obesity as a pharmacological condition rather than a behavioral one. Semaglutide doesn’t suppress appetite - it recalibrates the hedonic set point. The real tragedy isn’t the side effects, it’s that we’ve reduced human complexity to a single receptor agonist. We’re treating symptoms while ignoring systemic drivers: food deserts, chronic stress, sleep deprivation. This drug is a bandage on a hemorrhage.
And yet - I’d still prescribe it. Because sometimes, when the body is screaming, you need to silence the noise before you rebuild the house.
Anastasia Novak 6.01.2026
People are acting like this is some miracle cure when it’s basically just a chemical leash. You’re not ‘resetting’ your metabolism - you’re chemically numbing your hunger until you can’t even enjoy food anymore. And then you stop? Boom. Weight comes back like a vengeful ghost. This isn’t health. It’s pharmaceutical slavery. And the fact that people are calling this ‘empowerment’? Absolutely disgusting.
Jonathan Larson 6.01.2026
The clinical data on semaglutide is among the most robust in the history of obesity pharmacotherapy. Its efficacy in reducing adiposity, improving insulin sensitivity, and lowering systemic inflammation is not merely statistically significant - it is clinically transformative. However, the ethical imperative lies not in its mechanism, but in its accessibility. To deny a life-altering intervention due to cost or insurance policy is not merely a failure of healthcare - it is a moral failure of society. We treat hypertension with lifelong medication. We treat diabetes with lifelong medication. Why should obesity be any different?
Elen Pihlap 6.01.2026
wait so if i stop taking it i gain it all back??? omg i just started and i’m already obsessed with this stuff i can’t believe i’m gonna have to take this forever?? i just wanted to lose 10 lbs for my wedding and now i’m scared i’ll never be normal again 😭
Sai Ganesh 6.01.2026
When I was on Ozempic, I lost 28 pounds. But I also started cooking more, walking daily, and sleeping better. The drug didn’t do it alone. It gave me the mental space to build habits. I still take it two years later - not because I’m weak, but because my body needs it. Like insulin. Like blood pressure meds. This isn’t failure. It’s adaptation. And if society had better access, fewer people would feel ashamed for needing it.