Understanding Urinary Tract Infections and Kidney Stones
As a blogger who frequently discusses health issues, I have come across many cases of urinary tract infections (UTIs) and kidney stones. Today, I want to shed some light on the connection between these two common conditions. In this article, we will explore the causes, symptoms, and treatment options for both UTIs and kidney stones, and how they can be related to one another. So, let's dive into understanding the connection between urinary tract infections and kidney stones.
The Basics of Urinary Tract Infections
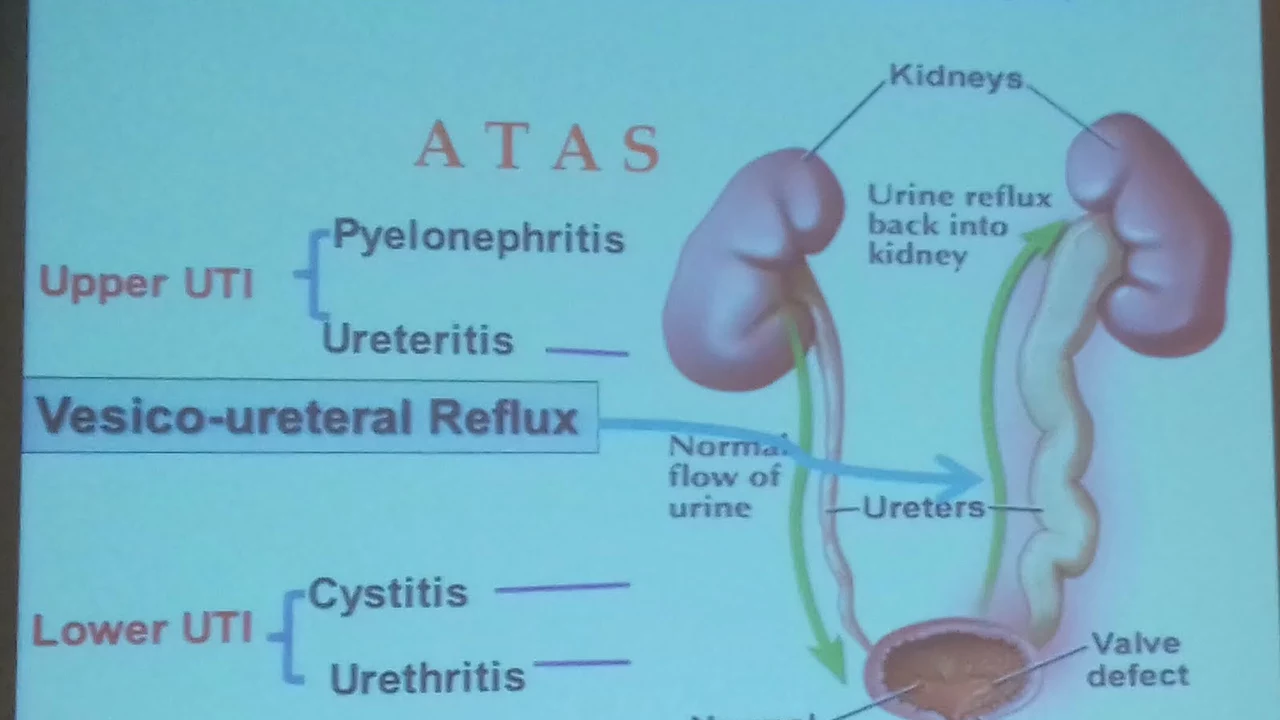
Urinary tract infections are bacterial infections that occur in any part of the urinary system, including the kidneys, bladder, ureters, and urethra. They are quite common, particularly among women, and can cause a range of uncomfortable symptoms. Some of the most common symptoms of UTIs include a strong, persistent urge to urinate, a burning sensation during urination, cloudy or strong-smelling urine, and lower abdominal pain.
UTIs are typically caused by bacteria entering the urinary tract through the urethra and then multiplying in the bladder. The most common type of bacteria responsible for UTIs is Escherichia coli (E. coli), which is usually found in the intestines. Risk factors for developing a UTI include being sexually active, using certain types of birth control, having a weakened immune system, and having a urinary tract abnormality.
What Are Kidney Stones?
Kidney stones are hard, mineral deposits that form inside your kidneys. They can vary in size and shape, and are often incredibly painful when they pass through the urinary tract. The symptoms of kidney stones include severe pain in the back or side, blood in the urine, nausea, vomiting, and frequent urination.
Kidney stones are formed when there is an excess of certain minerals in your urine, such as calcium, oxalate, and phosphorus. These minerals can combine and crystallize, forming stones. Factors that increase the risk of developing kidney stones include a family history of kidney stones, dehydration, obesity, and having a diet high in protein, sodium, and sugar.
The Connection Between UTIs and Kidney Stones
Now that we have a basic understanding of urinary tract infections and kidney stones, let's explore how these two conditions are connected. The primary connection between UTIs and kidney stones is that kidney stones can create an environment that is more conducive to bacterial growth and infection.
Kidney stones can cause blockages in the urinary tract, which can impede the flow of urine. This can lead to urine stagnation, creating a breeding ground for bacteria and increasing the risk of developing a UTI. In some cases, a UTI may even contribute to the formation of kidney stones by altering the chemical balance of the urine and promoting the crystallization of minerals.
Preventing and Treating UTIs and Kidney Stones
Understanding the connection between urinary tract infections and kidney stones is crucial for preventing and treating these conditions. Here are some tips for reducing your risk of both UTIs and kidney stones:
- Stay well-hydrated by drinking plenty of water throughout the day. This helps to dilute your urine and flush out bacteria and mineral deposits.
- Urinate frequently to help prevent the buildup of bacteria and minerals in your urinary tract.
- Maintain a healthy diet that is low in sodium, sugar, and excessive protein. This can help to reduce the risk of kidney stone formation.
- Practice good hygiene by wiping from front to back after using the toilet and washing your genital area before and after sexual activity.
- If you are prone to UTIs, consider using a different form of birth control, as some methods can increase the risk of infection.
If you suspect that you have a urinary tract infection or kidney stones, it is essential to seek medical attention as soon as possible. Your healthcare provider can diagnose your condition and recommend appropriate treatment options, which may include antibiotics for a UTI or pain relief and medical intervention for kidney stones.
Conclusion
In conclusion, urinary tract infections and kidney stones are indeed connected. Kidney stones can create an environment that promotes bacterial growth and infection, leading to UTIs. By understanding this connection, we can take steps to prevent and treat these conditions effectively. Remember to stay well-hydrated, practice good hygiene, and maintain a healthy diet to reduce your risk of both UTIs and kidney stones. And if you suspect you have either of these conditions, don't hesitate to seek medical help.

Émilie Maurice 18.06.2023
Kidney stones do not cause UTIs; they merely create conditions that can allow bacteria to thrive.
Veronica Mayfair 18.06.2023
Thanks for the thorough breakdown! I love how you highlighted staying hydrated 💧 and good hygiene 😊
Anthony Coppedge 18.06.2023
I appreciate your enthusiasm, and I must add, drinking ample water-at least two liters a day-is scientifically proven to dilute urine; furthermore, regular urination prevents bacterial stagnation, which in turn reduces infection risk; additionally, maintaining a balanced diet low in sodium and excessive protein supports renal health. Moreover, these preventive measures are universally recommended by urologists and nephrologists alike.
Joshua Logronio 18.06.2023
Watch out, the pharma giants don’t want you to know that staying hydrated is the real cure-they push pills instead.
Nicholas Blackburn 18.06.2023
That conspiracy nonsense is absurd; the evidence clearly shows that proper hydration and hygiene are the primary defenses, not some hidden agenda, and spreading such ideas only distracts from real medical advice.
Dave Barnes 18.06.2023
When we look at the relationship between urinary tract infections and kidney stones, the first thing to acknowledge is that both conditions share a common environment: the urinary system itself. A stone can obstruct flow, creating a pocket where urine stagnates, and that stagnant urine becomes a breeding ground for bacteria. Conversely, a persistent infection can alter the pH of the urine, making it easier for certain minerals to crystallize and form a stone. Research from several urology journals has documented cases where treating an infection reduced the recurrence of stones, suggesting a bidirectional influence. Hydration plays a pivotal role; drinking enough water not only flushes out tiny crystal precursors but also helps wash away bacteria before they can adhere to the bladder wall. Dietary choices matter as well-excessive salt can increase calcium excretion, while high animal protein can raise uric acid levels, both of which contribute to stone formation. On the other hand, sugary beverages may feed certain bacteria, leading to a higher incidence of UTIs, especially in women. Lifestyle habits such as regular physical activity improve overall metabolism and can help maintain a healthier urinary chemistry. For those prone to infections, prophylactic measures like cranberry supplements have shown modest benefits, though the evidence is mixed. In clinical practice, doctors often recommend a low‑oxalate diet alongside increased fluid intake to tackle both problems simultaneously. Patients with recurrent stones may undergo a metabolic work‑up to pinpoint specific abnormalities, such as hypercalciuria, which then guides personalized dietary advice. Similarly, individuals with frequent UTIs should be evaluated for underlying anatomical issues, like strictures or vesicoureteral reflux, that could also predispose them to stone formation. Medication choices matter too; some antibiotics can alter the gut microbiome, potentially influencing oxalate metabolism and stone risk. Therefore, a holistic approach that considers fluid intake, diet, medication, and even stress management tends to yield the best outcomes. It’s also worth noting that genetic factors can predispose certain people to both conditions, so family history should never be ignored. In summary, tackling UTIs and kidney stones together, rather than as isolated issues, offers a more efficient path to health and prevents a vicious cycle of recurring problems.
Kai Röder 18.06.2023
Thank you for such a comprehensive overview; I particularly appreciate the emphasis on personalized dietary plans and the reminder to assess underlying anatomical factors.
Brandi Thompson 18.06.2023
This article completely ignores the fact that most patients are non‑compliant with hydration recommendations and that the simplistic advice to drink more water is a lazy substitute for addressing the complex metabolic and genetic factors that truly drive stone formation and infection risk
Chip Hutchison 18.06.2023
I hear your concerns and agree that patient compliance is challenging, so we should also focus on behavioral strategies and supportive counseling to help people adopt healthier habits.