Chemotherapy isn’t a single drug. It’s a whole family of powerful chemicals designed to kill cancer cells by attacking the one thing they can’t control: their own speed. Cancer cells divide fast-too fast. And that’s exactly what chemotherapy exploits. It doesn’t care if you’re a healthy cell or a cancer cell. If you’re dividing quickly, you’re in the crosshairs. That’s why it works so well against tumors, and why it hits so hard on your hair, gut, and bone marrow.
How Chemotherapy Actually Kills Cancer Cells
There are more than 100 different chemotherapy drugs, but they all fall into six main groups, each with a different way of breaking down cell division. Alkylating agents like cyclophosphamide stick chemical groups onto DNA, making it impossible for the cell to copy itself. Think of it like gluing the pages of a book shut-no reading, no replication.
Antimetabolites, such as 5-fluorouracil and capecitabine, are imposters. They look like the building blocks cells need to make DNA and RNA, but once inside, they sabotage the process. The cell tries to use them, gets stuck, and dies. These are often used for colon and breast cancers.
Anthracyclines like doxorubicin do two things at once: they slip between DNA strands and block an enzyme called topoisomerase II that untangles DNA during division. The result? Broken DNA strands the cell can’t fix. This is why doxorubicin can turn your urine red-it’s just the drug passing through, not blood.
Plant alkaloids like vincristine and paclitaxel attack the cell’s skeleton. Cells need tiny structures called microtubules to pull chromosomes apart during division. Vincristine stops them from forming. Paclitaxel does the opposite-it locks them in place. Either way, the cell can’t split. Paclitaxel is given every three weeks at 175 mg/m² for breast cancer, a standard that’s held for over a decade.
Topoisomerase inhibitors like etoposide trap the enzyme that unwinds DNA, leaving it tangled and broken. And then there are miscellaneous agents-drugs that don’t fit neatly into the other groups but still wreck cancer cells in unique ways.
Most chemotherapy is given through an IV-about 65% of treatments. Oral pills like capecitabine make up 15%, and the rest are injected into the spinal fluid, abdomen, or arteries depending on the cancer’s location. Treatment happens in cycles: two to six weeks long, with a few days of drugs followed by rest. That rest isn’t just for you-it’s for your healthy cells to recover.
Why Chemotherapy Still Matters in 2025
You hear a lot about targeted therapies and immunotherapy now. They’re exciting. But chemotherapy is still the backbone. For acute myeloid leukemia (AML), it’s still first-line for 78% of patients. For ovarian cancer, nearly all patients get it. For colorectal cancer, it’s used in 85% of cases.
It’s also critical before surgery. In breast cancer, getting chemo first (neoadjuvant therapy) can shrink tumors enough to avoid mastectomies. In the SWOG S1418 trial, patients who achieved a pathologic complete response-meaning no cancer was found in the removed tissue-had significantly better survival. That’s not luck. That’s chemo working.
And it’s the only option for many. If your cancer doesn’t have a targetable mutation-like in many lung, pancreatic, or triple-negative breast cancers-chemotherapy is often the only tool that can reach every cell. Targeted drugs only work if the cancer has a specific glitch. Chemotherapy doesn’t care. It just attacks anything that divides fast.
The Side Effects: Not Just Nausea
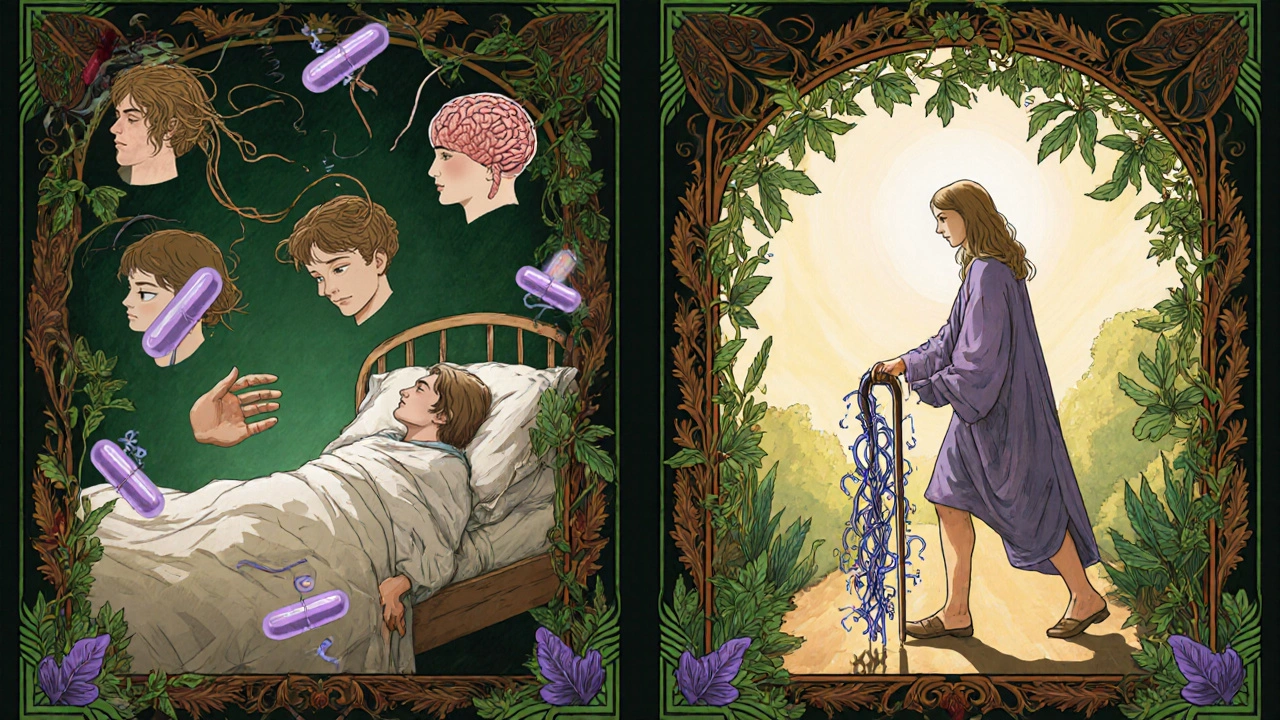
People think chemo side effects are just vomiting and hair loss. That’s only part of it. Fatigue hits 82% of patients. It’s not tiredness you can sleep off. It’s a deep, bone-aching exhaustion that lingers for weeks. Many say it’s worse than the nausea.
Hair loss affects 78%. It’s not just the scalp. Eyebrows, eyelashes, underarms, legs-everything can go. Scalp cooling caps now reduce this to about 25% for some drugs like taxanes, but they’re not perfect. And they’re not covered by insurance everywhere.
Nausea has gotten better, thanks to drugs like ondansetron. In the 1990s, 70-80% of patients had severe vomiting. Now, it’s down to 10-20% for the worst regimens. But delayed nausea-hitting 24 hours or more after treatment-is still a problem. Only 32% of patients find anti-nausea meds helpful for that.
Then there’s chemo brain. It’s real. About 75% of patients report trouble focusing, remembering names, or multitasking during treatment. One in three still feel it six months after finishing. Meditation apps like Calm or Headspace, used 20 minutes a day, have been shown to cut cognitive complaints by 40%. It’s not a cure, but it helps.
Peripheral neuropathy-tingling, burning, or numbness in hands and feet-happens in 30-40% of people on taxanes or platinum drugs. For 5-10%, it never goes away. Doctors now tell patients to avoid cold drinks, wear gloves when handling things, and report symptoms early. Waiting too long can mean permanent nerve damage.
And then there’s the silent stuff: low white blood cells (neutropenia). A fever of 100.4°F or higher during chemo is a medical emergency. You can’t wait. You go to the ER. That’s because your immune system is down. Your body can’t fight off even a common cold.
What Actually Helps With Side Effects
There’s no magic pill for chemo fatigue. But exercise works. Thirty minutes a day of walking or light cycling reduces fatigue by 25-30%, according to 17 clinical trials. You don’t need to run a marathon. Just move.
Hydration helps mild fatigue and diarrhea. Drink 1 to 2 liters of water daily. It sounds simple, but when you’re nauseated, it’s hard. Sipping ice chips or sucking on frozen grapes can help.
For nausea, eat small, bland meals. Toast, bananas, rice, crackers. Avoid greasy, spicy, or sweet foods. Eat before the chemo hits, not after. And keep dexamethasone pre-meds in mind-they reduce inflammation but can wreck your sleep. Many patients report severe insomnia from them.
For mouth sores, use a soft toothbrush and saltwater rinses. Avoid alcohol-based mouthwashes. For diarrhea, Imodium can help-but only if it’s not caused by infection. Always check with your team first.
And for neuropathy? Avoid ice packs. Don’t walk barefoot. Test water temperature before showering. Use oven mitts. These aren’t small tips. They’re safety measures to prevent burns or falls.
What’s New in 2025
Chemotherapy isn’t standing still. In June 2023, the FDA approved trilaciclib (Cosela), the first drug designed to protect bone marrow during chemo. It’s used for small cell lung cancer and helps keep white blood cell counts higher, reducing infections and the need for transfusions.
Medical cannabis is getting more attention. A 2023 study showed CBD and THC combinations reduced neuropathic pain by 55% in chemo patients. It’s not yet standard, but clinics in some states are starting to offer it.
Scalp cooling systems are now in the National Comprehensive Cancer Network’s 2024 guidelines. Used during taxane treatments, they lower hair loss from 65% to 25%. They’re expensive and not always covered, but for many, it’s worth it.
And the big picture? Chemotherapy isn’t being replaced-it’s being paired. More and more, it’s used with immunotherapy. For example, in lung cancer, chemo + checkpoint inhibitors now outperform chemo alone. It’s not either/or anymore. It’s both.

What Patients Say
On Reddit’s r/cancer, one patient wrote: "I could manage the physical side effects, but the cognitive changes made me feel like I wasn’t myself." Another said: "The Imodium worked for my diarrhea, but nothing helped the metallic taste. It felt like I was chewing aluminum foil."
These aren’t rare complaints. They’re everyday realities. But patients also say this: "The nausea control now is nothing like it was 15 years ago." And: "My nurse taught me how to track my symptoms. That made all the difference."
By the third cycle, 85% of patients figure out what works for them. It’s not about being strong. It’s about being smart. Knowing your triggers. Knowing when to call your doctor. Knowing that some side effects are normal, and others are urgent.
Is Chemotherapy Right for You?
It’s not always the answer. For some prostate cancers, hormone therapy works better with fewer side effects. For HER2-positive breast cancer, targeted drugs like Herceptin are often first. But for the majority of cancers-especially those that spread or grow fast-chemotherapy remains essential.
The goal isn’t to live forever. It’s to live well. To shrink the tumor. To give you time. To give you a shot. And in many cases, that shot still comes in the form of a drip, a pill, or an injection.
Chemotherapy isn’t pretty. But it’s powerful. And in 2025, it’s smarter than ever. Better scheduling. Better supportive care. Better combinations. It’s not the future of cancer treatment. But it’s still the present-and for millions, it’s the reason they’re still here.
How long does chemotherapy stay in your body?
Most chemotherapy drugs leave your body within 24 to 48 hours through urine, stool, or sweat. But the side effects can last much longer. Fatigue, nerve damage, or cognitive changes may linger for months or even years. The drug is gone, but the impact isn’t always.
Can you work during chemotherapy?
Many people do, but it depends on the treatment, the job, and how your body reacts. Fatigue and chemo brain are the biggest barriers. Some patients work part-time, from home, or on flexible hours. Employers are legally required to make reasonable accommodations under disability laws. Talking to your oncology team and HR early helps.
Do all chemotherapy drugs cause hair loss?
No. Some drugs, like capecitabine or temozolomide, rarely cause hair loss. Others, like doxorubicin or paclitaxel, almost always do. It depends on the drug, the dose, and how it’s given. Scalp cooling can help reduce hair loss for certain regimens, especially with taxanes.
Is chemotherapy more effective than radiation?
They’re different tools. Radiation targets one area-like a tumor in the breast or lung. Chemotherapy travels through your whole body. If cancer has spread, chemo is usually better. If it’s localized, radiation might be enough-or used with chemo for better results. Often, they’re combined.
Can you drink alcohol while on chemotherapy?
It’s usually not recommended. Alcohol can worsen dehydration, irritate your mouth and gut, and interfere with how your liver processes chemo drugs. Some drugs, like methotrexate, become more toxic with alcohol. Always check with your oncologist. A glass of wine occasionally might be okay, but don’t assume it is.
What should you do if you miss a chemotherapy dose?
Don’t double up. Call your oncology team immediately. Chemotherapy schedules are carefully timed to balance effectiveness and safety. Missing a dose can reduce the treatment’s impact or increase side effects. Your team will adjust based on the drug, your health, and how much time has passed.
Are there foods to avoid during chemotherapy?
Yes. Avoid raw or undercooked meats, eggs, and seafood-your immune system is weaker. Skip unpasteurized cheeses and juices. Limit sugar and processed foods-they don’t feed cancer, but they can worsen inflammation and fatigue. Focus on protein, vegetables, and hydration. Small, frequent meals are easier to handle than three big ones.
Can chemotherapy cure cancer?
In some cases, yes. For testicular cancer, Hodgkin lymphoma, and some leukemias, chemotherapy can lead to complete, lasting remission. For others, like advanced breast or lung cancer, it may not cure-but it can extend life by years, sometimes with good quality. The goal changes based on the cancer stage and type. It’s not always about cure. Sometimes, it’s about control.

Denny Sucipto 17.11.2025
Man, I remember when my mom went through chemo. The fatigue? Like carrying a fridge around all day. But she started walking 20 minutes after breakfast-just around the block-and it changed everything. Not magic, just motion. She said it made her feel like she wasn’t just a patient anymore.
Christine Eslinger 17.11.2025
It’s wild how much we’ve improved since the 90s. Back then, nausea was a rite of passage. Now we’ve got antiemetics that actually work, scalp cooling that’s gaining traction, and even trilaciclib protecting bone marrow. It’s not perfect, but we’re finally treating the whole person-not just the tumor.
And chemo brain? Real. Not ‘just stress.’ Studies show it’s neuroinflammation. Meditation helps because it lowers cortisol. Not a cure, but a bridge. Small wins matter.
Hydration isn’t just ‘drink water.’ It’s sipping frozen grapes when your mouth feels like sandpaper. It’s knowing your body’s new language. And that’s wisdom.
People think chemo is brute force. It’s not. It’s precision. Timing. Cycles designed to give healthy cells breathing room. That’s science, not cruelty.
The fact that we’re pairing it with immunotherapy now? That’s the future. Not replacement. Evolution.
And yes, some side effects linger. But so do people. And that’s the point.
Holly Powell 17.11.2025
Let’s be real-chemotherapy is a 1940s solution with a 2025 paint job. They still use alkylating agents that damage DNA indiscriminately? That’s not medicine, it’s arson with a prescription. And don’t get me started on the profit margins. Big Pharma loves chemo because it’s repeatable, expensive, and patients are too desperate to question it.
Scalp cooling? A Band-Aid. CBD? A distraction. They’re not fixing the system-they’re just making the suffering slightly more marketable.
If you want real progress, stop glorifying a treatment that turns people into walking side effect lists.
Heidi R 17.11.2025
Ugh, I hate when people act like chemo is ‘brave’ or ‘strong.’ It’s not a character test. It’s a biological assault. And the way we romanticize it? Toxic.
‘You’re so strong!’ No. I’m chemically neutered and tired. Stop thanking me for surviving your version of hell.
Emanuel Jalba 17.11.2025
Y’all need to stop normalizing this. 😔 Chemotherapy is basically poisoning your body to kill something that’s already poisoning it. 😡 Like, why not just let nature take its course? 🤔 I saw a documentary-cancer cells are just your own cells going rogue because of toxins in the environment. 🌱 So why are we attacking the host? 🤯
And why are they NOT talking about the glyphosate? 🚫🌾 Or the PFAS in your water? 🚿
Chemo’s just a band-aid on a nuclear reactor. 🔥
Kristina Williams 17.11.2025
They’re lying about the 24-hour clearance. I tested my pee after chemo. Still had traces at 72 hours. And the ‘safe’ urine? They don’t tell you your partner can get exposed. I read the safety sheets-there’s a whole section on ‘avoid contact with bodily fluids.’ But no one says it out loud. 😷
And the ‘no alcohol’ rule? My oncologist said ‘a glass is fine’ but the nurse whispered, ‘Don’t tell anyone.’
They’re hiding stuff.
Girish Pai 17.11.2025
Let’s cut through the fluff. Chemotherapy remains the most cost-effective cytotoxic intervention globally, especially in resource-limited settings. Targeted therapies? Exorbitant. Immunotherapies? Require biomarker stratification, which is not scalable in low-income countries. In India, we administer 5-FU and cisplatin as backbone regimens for esophageal and cervical cancers-survival gains are statistically significant. The infrastructure for precision medicine is still nascent. Chemo is not outdated-it’s equitable.
Also, paclitaxel dosing at 175 mg/m² every 3 weeks? That’s NCCN-class I evidence. Not opinion. Fact.
Kristi Joy 17.11.2025
My sister got chemo for stage 3 breast cancer. She didn’t lose her hair-used a cooling cap. But the neuropathy? She couldn’t button her shirt for months. We bought those grip gloves. The kind you use for gardening. Helped her hold a fork again.
And the fatigue? She didn’t push through it. She scheduled naps like meetings. ‘3 p.m. rest. No apologies.’ That’s the real hack: treating recovery like part of the treatment.
Also-yes, the metallic taste is real. I made her smoothies with pineapple and mint. It masked it better than anything.
Shilpi Tiwari 17.11.2025
Interesting breakdown of drug classes. I’d add that antimetabolites like capecitabine are prodrugs-activated intracellularly by thymidine phosphorylase, which is overexpressed in many tumors. That’s why they’re selectively toxic. The tumor essentially turns the drug into its own poison.
Also, topoisomerase II inhibitors induce double-strand breaks. That’s why anthracyclines carry that black box warning for cardiotoxicity-ROS generation in cardiac myocytes. Mitochondrial damage.
And trilaciclib? It’s a CDK4/6 inhibitor that transiently arrests hematopoietic stem cells in G1, shielding them from S-phase cytotoxics. Elegant mechanism. Not just ‘protection’-it’s cell cycle manipulation.
Still, the psychosocial burden remains grossly understudied.
Louie Amour 17.11.2025
You people act like chemo is some noble sacrifice. It’s not. It’s a gamble with your organs. Liver, kidneys, heart-you’re trading long-term function for short-term tumor shrinkage. And for what? A 5% survival bump? That’s not hope. That’s statistical theater.
I’ve seen patients on 3rd-line chemo, bald, dialysis-dependent, still getting IVs because ‘we don’t want to give up.’
That’s not medicine. That’s institutional denial.
And don’t get me started on the ‘you’re so brave’ comments. I’d rather be dead than hear that again.
Shaun Barratt 17.11.2025
Apologies for the typo in my previous comment (I meant ‘cytotoxic’ not ‘cytotoxics’). The data on chemo-induced cognitive decline is robust-fMRI studies show reduced connectivity in the prefrontal cortex during treatment. This is not ‘brain fog’-it’s neurostructural change. The fact that we don’t screen for it routinely is a systemic failure.
Also, the 2024 NCCN scalp cooling guidelines were based on a meta-analysis of 12 RCTs with over 2,000 patients. The OR for hair preservation was 3.8 (95% CI: 2.9–5.1). This is not anecdotal. It’s evidence-based.
But yes, cost and access remain critical barriers.
Brenda Kuter 17.11.2025
They don’t tell you about the shame. 😭 You sit there, hooked up to the drip, and everyone’s like, ‘You look great!’ But you feel like a ghost. Your hair’s gone, your nails are crumbling, and you’re scared to look in the mirror. 😔
And then your coworker says, ‘I heard if you eat turmeric, it kills cancer!’ 🤦♀️
And your mom cries every time you leave the house. 🥺
It’s not the chemo that breaks you. It’s the silence after the ‘you’re so strong’ comments. 🫂
Hal Nicholas 17.11.2025
Let’s be honest-chemotherapy is the last resort for doctors who don’t want to admit they don’t know what else to do. You’ve got this whole elaborate system built on fear: ‘If you don’t do chemo, you’ll die.’ But what if you die anyway? What if you just spend your last months vomiting in a hospital bed?
I’ve seen too many people get chemo at 80 with metastatic cancer. They don’t live longer. They just live sadder.
And the ‘it’s smarter now’ narrative? It’s propaganda. They’re just putting new labels on old poison.
Real medicine doesn’t require you to lose your identity to survive.