Bronchodilator Selector Tool
Quick Takeaways
- Bronchodilators relax airway muscles, making it easier to breathe during a bronchitis flare‑up.
- Short‑acting beta‑agonists (SABAs) are preferred for sudden symptom relief; long‑acting beta‑agonists (LABAs) are used only when bronchitis becomes chronic.
- Anticholinergics work well for cough‑dominant bronchitis and can be combined with SABAs.
- Inhaler technique matters more than the drug itself - poor technique wastes medication and prolongs recovery.
- Side‑effects are usually mild, but over‑use can lead to tachycardia, tremor, or worsening airway inflammation.
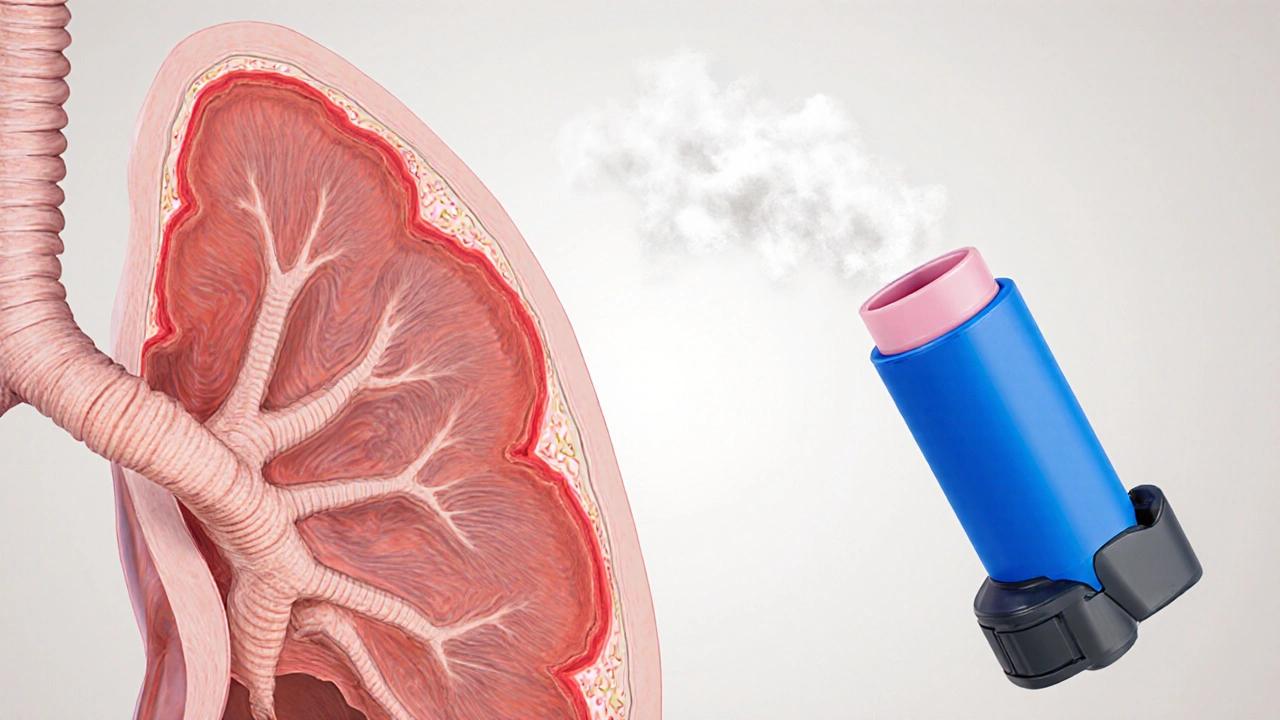
When you hear the word bronchodilators, you probably picture a bright‑colored inhaler sitting on a nightstand. In reality, a bronchodilator is any medication that widens the airways by relaxing the smooth‑muscle ring around them. For people battling bronchitis - an inflammation of the bronchial tubes that often brings coughing, mucus, and shortness of breath - those drugs can be a game‑changer. Below we’ll break down why, when, and how to use them safely.
Bronchodilator is a medication class that relaxes airway smooth muscle, increasing airflow and reducing breathlessness. Bronchitis is a inflammatory condition of the bronchial tubes, typically caused by viruses, bacteria, or irritants such as smoke.How bronchodilators actually work
Think of the airway like a garden hose. When the hose narrows, water pressure drops and you can’t water the plants efficiently. Bronchodilators act like a garden‑hose widener - they loosen the muscular wall (the “valve”) around the airway, allowing more air to flow through.
The two main pathways they target are:
- Beta‑adrenergic receptors: Stimulating these receptors (with beta‑agonists) tells the muscle to relax quickly.
- Muscarinic receptors: Blocking these (with anticholinergics) stops the muscle from tightening.
Both pathways reduce airway resistance, but they differ in speed, duration, and side‑effect profile. That’s why doctors match the drug to the patient’s specific bronchitis pattern.
Common bronchodilator types used for bronchitis
Below is a snapshot of the most frequently prescribed options. The table includes onset (how fast you feel relief), typical duration, and a real‑world brand example.
| Type | Onset | Duration | Typical Use in Bronchitis | Example Drug |
|---|---|---|---|---|
| Short‑acting beta‑agonist (SABA) | 1-5minutes | 4-6hours | Acute symptom relief during flare‑ups | Albuterol (Ventolin) |
| Long‑acting beta‑agonist (LABA) | 15-30minutes | 12hours or more | Maintenance for chronic bronchitis or COPD overlap | Salmeterol (Serevent) |
| Anticholinergic (LAMA) | 5-15minutes | 24hours | Supplement SABA when cough is dominant; useful in smokers | Tiotropium (Spiriva) |
| Combination (SABA+LAMA) | 1-5minutes | 12-24hours | Severe acute bronchitis with poor response to single agents | Formoterol/Budesonide (Symbicort) - note the steroid component |

When to reach for a bronchodilator
Bronchitis comes in two flavors: acute (usually viral, lasting <3weeks) and chronic (often linked to smoking or long‑term irritants). The decision to prescribe a bronchodilator hinges on three factors:
- Severity of airway narrowing: Wheezing, audible chest tightness, or a measurable drop in peak flow suggests a need for a bronchodilator.
- Speed of symptom progression: Sudden worsening calls for a fast‑acting agent (SABA). Gradual decline may benefit a maintenance LABA.
- Co‑existing conditions: Asthma, COPD, or heart disease influence drug choice. For example, patients with cardiac arrhythmias may tolerate anticholinergics better than high‑dose SABAs.
In practice, most primary‑care doctors start with a SABA inhaler for acute bronchitis. If the patient reports frequent nighttime coughing that disrupts sleep, a low‑dose inhaled corticosteroid (ICS) may be added, but the bronchodilator remains the first line for immediate relief.
Benefits you can expect
When used correctly, bronchodilators can:
- Reduce coughing episodes by opening high‑airflow pathways.
- Improve oxygen saturation, which speeds up tissue healing.
- Lower the risk of secondary bacterial infection caused by mucus stasis.
- Shorten the overall duration of an acute bronchitis episode by 1-2days (studies from 2023‑2024 report a 15% reduction).
Those gains matter especially for older adults who might otherwise face hospitalization.
Potential side‑effects and how to avoid them
Every medication has a trade‑off. Common side‑effects for bronchodilators include:
- Tremor or shaky hands - usually transient, resolves within 30minutes.
- Rapid heartbeat (tachycardia) - higher doses of SABAs can trigger this; keep rescue‑inhaler use under 4 puffs per 24hours.
- Dry mouth - anticholinergics are notorious for this; sipping water after each puff helps.
- Paradoxical bronchospasm - rare, but if breathing worsens right after a puff, stop and contact a clinician.
Key strategies to keep risks low:
- Follow the prescribed dose - more isn’t better.
- Use a spacer or holding chamber with metered‑dose inhalers (MDIs) to improve deposition.
- Routinely check peak‑flow readings if you have a home meter; a sudden dip signals over‑use or worsening disease.

Getting the most out of your inhaler
Even the best bronchodilator is useless if you can’t get the drug into your lungs. Here’s a step‑by‑step for a standard MDI:
- Shake the inhaler for 5seconds.
- Exhale fully, away from the mouthpiece.
- Place the mouthpiece between your teeth, close your lips around it.
- Press down once while starting a slow, steady inhalation.
- Hold your breath for about 10seconds, then exhale slowly.
- If a second puff is prescribed, wait 30seconds before repeating.
Dry‑powder inhalers (DPIs) skip the shaking step but require a fast, deep breath. Use a spacer with MDIs if you have hand‑tremor or arthritis - it reduces coordination demands.
Special considerations for different groups
Children (under 12): SABAs are safe, but dosing is weight‑based. Use a child‑size mask with the inhaler if the child can’t coordinate breathing.
Pregnant women: Short‑acting bronchodilators are categoryB (low risk) and can be used when bronchitis symptoms threaten oxygenation.
Elderly: Start with the lowest effective dose; many older adults have co‑existing heart disease that makes high‑dose SABAs risky.
Alternatives and adjuncts
If bronchodilators aren’t enough, doctors may add:
- Oral antibiotics - only when a bacterial superinfection is confirmed.
- Inhaled corticosteroids (ICS) - to reduce underlying inflammation, especially in chronic bronchitis.
- Chest physiotherapy - percussion or vibration to loosen mucus.
- Hydration and humidified air - simple but effective at thinning secretions.
These aren’t replacements for bronchodilators; they work best when combined.
Frequently Asked Questions
Can I use a bronchodilator for a cold?
A common cold can cause mild bronchial irritation, but bronchodilators are only recommended if you develop wheezing or shortness of breath. Otherwise, rest, fluids, and over‑the‑counter decongestants are sufficient.
How many puffs of albuterol are safe per day?
Most guidelines cap rescue‑inhaler use at 4-6 puffs in a 24‑hour period. Exceeding that suggests uncontrolled disease and warrants a doctor’s review.
Do bronchodilators cure bronchitis?
No. They relieve airway narrowing and improve airflow, but the underlying inflammation still needs time to heal. In chronic cases, they serve as long‑term maintenance.
Is it okay to use a spacer with a dry‑powder inhaler?
Spacers are designed for MDIs. Using one with a DPI can actually reduce drug delivery because DPIs rely on the inspiratory flow directly into the device.
Can over‑use of bronchodilators cause more mucus production?
Excessive SABA use may dry out the airway lining, which can thicken mucus temporarily. Staying within prescribed limits and drinking water after each use helps keep secretions thin.

Megan Lallier-Barron 5.10.2025
While most people think bronchodilators are just a quick fix, they actually bridge the gap between a cough and real breathability 😊. Think of them as the unsung diplomats of your airway, negotiating peace between muscle and airflow. The selector tool is handy, but remember the human factor-technique matters more than the molecule.
Kelly Larivee 5.10.2025
Bronchodilators help open up the airways fast, especially when you feel tight. Just use the inhaler correctly and you’ll notice relief sooner.
Emma Rauschkolb 5.10.2025
From a pharmacodynamic standpoint, SABAs activate β2‑adrenergic receptors, increasing intracellular cAMP and causing smooth‑muscle relaxation :) . In chronic cases, LABAs sustain this effect, reducing exacerbation frequency. Anticholinergics, meanwhile, block muscarinic receptors, curbing bronchoconstriction. Misusing these agents can lead to tachyphylaxis, so cycle them wisely.
Kaushik Kumar 5.10.2025
Listen up!!! If you’re battling breathlessness, you need a plan-assessment, proper inhaler technique, and a follow‑up schedule!!! The tool gives you a starting point, but don’t forget regular check‑ins with your provider-yes, those appointments matter!!!
Mara Mara 5.10.2025
Our country's best doctors swear by using inhalers correctly!
Jennifer Ferrara 5.10.2025
In the clinical management of bronchitis, bronchodilators represent a cornerstone of symptomatic therapy, particularly when airway obstruction is evident. The underlying mechanism involves the activation of β2‑adrenergic receptors, which elicits relaxation of bronchial smooth muscle and consequent reduction in airway resistance. Moreover, anticholinergic agents impede the action of acetylcholine on muscarinic receptors, thereby diminishing bronchoconstriction. It is imperative to differentiate between short‑acting agents, such as albuterol, which provide rapid relief, and long‑acting formulations like salmeterol, intended for maintenance therapy. Evidence suggests that inappropriate reliance on short‑acting bronchodilators without addressing the inflammatory component may lead to suboptimal outcomes. Consequently, clinicians often combine bronchodilators with inhaled corticosteroids to achieve both bronchodilation and anti‑inflammatory effects. Patients should be educated on correct inhaler technique, as poor coordination can result in reduced drug deposition and unnecessary dose escalation. The selector tool outlined in the article serves as a useful adjunct, yet it cannot substitute for individualized clinical judgment. Additionally, healthcare providers must monitor for adverse events, such as tachycardia, tremor, and paradoxical bronchospasm, particularly in patients with comorbid cardiac conditions. Regular spirometric assessment can aid in tracking therapeutic response and adjusting medication regimens accordingly. While the tool recommends combinations for smokers, clinicians should also prioritize smoking cessation counseling as a fundamental intervention. Finally, documentation of medication adherence and side‑effect profile remains essential for optimizing long‑term management of chronic bronchitis. In sum, bronchodilators, when employed judiciously and in concert with comprehensive care, markedly improve patient quality of life. Future research may elucidate novel receptor pathways that could further refine therapy. Until then, adherence to established guidelines remains the best practice.
Terry Moreland 5.10.2025
It’s easy to feel overwhelmed when the inhaler instructions look like a cryptic manual, but take it step by step. A good rule of thumb is to exhale fully, seal your lips, and then inhale slowly while activating the device. If you practice daily, the technique becomes second nature and you’ll get the full benefit.
Abdul Adeeb 5.10.2025
From a pharmacological perspective, the distinction between β‑agonists and anticholinergics lies in receptor selectivity, which influences both onset and duration of action. Accordingly, clinicians tailor therapy based on symptom predominance and patient history.
Abhishek Vernekar 5.10.2025
Hey there! If you notice your breathlessness creeping up, a quick puff of a SABA can bring you back to normal in minutes. Just keep an eye on usage, and talk to your doctor if you need more than two doses a day.
lalitha vadlamani 5.10.2025
One must not cavalierly dismiss the gravity of inhaler misuse; the ramifications extend beyond mere discomfort. In the theater of respiratory health, bronchodilators are the protagonists, yet their performance falters without proper direction. Thus, the onus lies with both practitioner and patient to rehearse technique diligently. Neglect, however, invites an unwelcome climax of exacerbation.
Matthew Moss 5.10.2025
American physicians have pioneered inhaler technology, and it’s high time we trust home‑grown solutions over foreign alternatives. Simplicity and effectiveness are hallmarks of our own formulations, and patients should prioritize them.
Antonio Estrada 5.10.2025
When deciding between a SABA and a LAMA, consider whether the cough or the breathlessness is more limiting. Combining both can be worthwhile for severe cases, but always align with a physician’s guidance. Sharing experiences in support groups also helps fine‑tune personal regimens.
Sumeet Kumar 5.10.2025
Stay positive! 🌟 Proper inhaler use can dramatically improve your daily life, and the selector tool is a great starting point. Keep practicing, and celebrate each breath of relief! 😊
Maribeth Cory 5.10.2025
Don’t let the learning curve intimidate you; mastery comes with consistent practice. Reach out to a respiratory therapist if you need a hands‑on refresher.
andrea mascarenas 5.10.2025
Good technique matters more than the brand you pick. Keep it simple and follow the steps.
Camille Ramsey 5.10.2025
Yo, dont think u can just spray any inhaler and be cool. The tool tells u wut 2 use, so stop guessin and read the labels.
Scott Swanson 5.10.2025
Oh great, another “quick fix” gadget-because we all love a one‑size‑fits‑all inhaler, right? Spoiler: it only works if you actually use it correctly.
Karen Gizelle 5.10.2025
Honestly, I’ve seen too many patients blame their symptoms on “the inhaler” without checking technique first. It’s a classic case of the “blame the tool” fallacy. Proper education can prevent endless cycles of unnecessary prescriptions. Also, remember that over‑reliance on SABAs may mask underlying issues. So, keep the conversation open with your doctor.