Fournier's Gangrene Symptom Checker
Critical Warning Signs
Fournier's gangrene is a medical emergency. If you experience any of these symptoms while taking SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin), go to the emergency room immediately.
Every hour of delay increases your risk of death by about 9%.
Do you have any of these symptoms?
Critical Action Required
EMERGENCY ALERT
You have symptoms of Fournier's gangrene. This is a medical emergency.
No Emergency Symptoms Detected
Based on your responses, no urgent symptoms of Fournier's gangrene are present. However:
- Know the signs: Stay vigilant for sudden severe pain, rapid swelling, or skin discoloration.
- Prevention: Keep blood sugar controlled (HbA1c <7%), practice good hygiene, and report recurring infections to your doctor.
- Important: Do not stop your SGLT2 inhibitor without consulting your doctor.
When you’re managing type 2 diabetes, taking a medication like canagliflozin, dapagliflozin, or empagliflozin can feel like a win. These drugs - known as SGLT2 inhibitors - help your kidneys flush out extra sugar through urine, lowering blood glucose and offering real protection for your heart and kidneys. But there’s a rare, serious side effect you need to know about: Fournier’s gangrene. It’s not common. But when it happens, it moves fast. And if you don’t act immediately, it can be deadly.
What Is Fournier’s Gangrene?
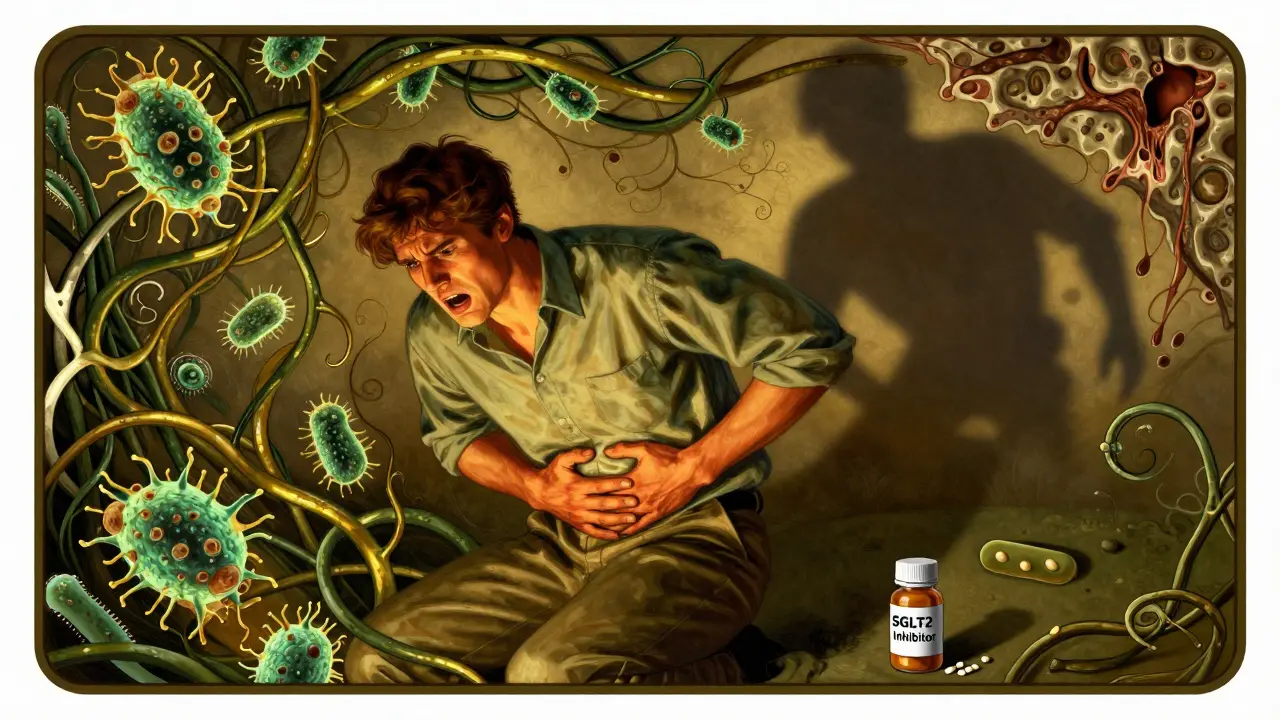
Fournier’s gangrene is a rare but deadly bacterial infection that eats away at the skin and tissue around your genitals, perineum, or anus. It’s a type of necrotizing fasciitis - the so-called "flesh-eating" infection - but it’s localized to the lower body. It doesn’t start with a cut or scrape. It begins quietly: a dull ache, a patch of redness, a feeling that something’s "off." Within hours, it can explode into swelling, fever, and intense pain. Skin turns dark, blisters form, and tissue dies. The infection spreads through the layers of tissue, and without emergency treatment, it can reach your bloodstream and shut down your organs.Why Do SGLT2 Inhibitors Increase the Risk?
SGLT2 inhibitors work by blocking glucose reabsorption in the kidneys. That means extra sugar leaves your body through urine. Sounds good - until that sugar becomes a feast for bacteria. The warm, moist environment around your genitals becomes a breeding ground. Bacteria like E. coli, Klebsiella, and even anaerobes thrive on that sugar. The glucose in your urine doesn’t just feed them - it may also weaken local defenses by altering pH and tissue hydration. Studies show nearly all reported cases involved people with diabetes who had poor blood sugar control. So it’s not just the drug. It’s the combo: high sugar in urine + high blood sugar + a weakened immune system.Who’s at Risk?
The risk is low - about 1 in 10,000 men taking these drugs over a few years. But it’s not zero. And it’s not just men. While 70% of cases are in men, nearly one-third of reported cases in Europe were in women. You’re at higher risk if:- You have HbA1c above 9%
- You’ve had recurrent genital yeast infections (thrush) before starting the drug
- You have a weakened immune system from other conditions or medications
- You’re obese or have poor hygiene
- You have a history of urinary tract infections or catheter use
Even if you don’t fit these categories, you still need to know the signs. Because this doesn’t wait for permission.

Early Warning Signs You Can’t Ignore
This isn’t a rash or a mild irritation. Fournier’s gangrene doesn’t come with a warning label. It strikes suddenly. Here’s what to look for - and don’t wait for all of them:- Severe pain in the genitals, anus, or inner thighs - worse than any infection you’ve had before
- Swelling that gets worse over hours, not days
- Redness or purple discoloration of the skin that spreads quickly
- Fever above 38°C with chills or feeling extremely unwell
- Crackling sensation under the skin when touched - this means gas from bacteria
- Dead tissue - skin turning black, gray, or necrotic
- Foul-smelling discharge from the area
If you’re on an SGLT2 inhibitor and notice even one of these - especially pain and swelling - go to the emergency room now. Don’t call your doctor. Don’t wait until morning. Don’t assume it’s just a yeast infection again. This is different. This is urgent.
What to Do If You Suspect Fournier’s Gangrene
There’s no home remedy. No over-the-counter cream. No waiting it out. Here’s what happens next:- Stop the SGLT2 inhibitor immediately. Do not take another dose. Even if you’re not sure - stop.
- Go to the nearest emergency department. Tell them you’re on an SGLT2 inhibitor and suspect Fournier’s gangrene. Say the name. Don’t say "it hurts down there." Say the condition. It saves time.
- Expect immediate action. Doctors will order blood tests, imaging (CT or MRI), and start broad-spectrum antibiotics right away - often within an hour.
- Surgery is almost always needed. Surgeons will cut away dead tissue. This isn’t optional. It’s life-saving. Multiple surgeries may be required.
Every hour of delay increases your risk of death by about 9%. If treatment starts within 24 hours, survival rates jump from under 50% to over 80%. Speed isn’t just important - it’s everything.
Regulators and Doctors Are Watching
The FDA added a boxed warning to all SGLT2 inhibitors in 2018 - the strongest possible alert. The European Medicines Agency and the UK’s MHRA did the same. They didn’t pull the drugs. They didn’t say "don’t use them." They said: "Know the signs. Act fast. The benefits still outweigh the risks for most people."Since 2018, more cases have been reported. But the number of people taking these drugs has also grown - over 10 million globally. The rate? Still about 1.9 cases per 100,000 patient-years. That’s rarer than being struck by lightning. But the consequences? Not rare at all.
Should You Stop Taking Your SGLT2 Inhibitor?
No - unless you’re having symptoms. These drugs do more than lower blood sugar. They reduce your risk of heart failure, hospitalization, and kidney failure. For people with heart disease or chronic kidney disease, they’re life-extending. Stopping them without a reason puts you at greater risk than the rare chance of Fournier’s gangrene.But here’s what you should do:
- Get educated. Know the signs. Show your partner or family what to look for.
- Keep your blood sugar under control. HbA1c below 7% lowers your risk significantly.
- Practice good hygiene. Wash daily, dry thoroughly, change underwear often.
- Don’t ignore genital itching or recurring infections. Tell your doctor. You might need a different medication.
- If you’ve had genital infections before starting SGLT2 inhibitors, talk to your doctor about alternatives like GLP-1 agonists.
What If You’ve Already Had a Genital Infection?
If you’ve had two or more yeast infections or urinary tract infections since starting your SGLT2 inhibitor, talk to your doctor. It’s not a reason to panic - but it is a reason to reassess. Your doctor might switch you to another class of drug, like a GLP-1 agonist (such as semaglutide or liraglutide), which has no known link to Fournier’s gangrene. These drugs also protect your heart and kidneys - just differently.There’s no shame in switching. Your health isn’t about sticking with the first pill you were given. It’s about staying alive and well.
What’s Next?
Researchers are now building risk scores to predict who’s most likely to develop Fournier’s gangrene on SGLT2 inhibitors. Factors like HbA1c, BMI, infection history, and immune status will help doctors decide who gets these drugs - and who doesn’t. For now, the message is simple: know the signs. Act fast. Don’t wait.If you’re on one of these medications, you’re not alone. Millions are. Most will never face this complication. But if you’re the one in 10,000 - your awareness could save your life.
Can women get Fournier’s gangrene from SGLT2 inhibitors?
Yes. While most cases occur in men, about one-third of reported cases in Europe were in women. The mechanism is the same: glucose in urine creates a bacterial breeding ground. Any person with a genital or perineal area is at risk. Women should not assume they’re immune.
Is Fournier’s gangrene the same as a yeast infection?
No. Yeast infections cause itching, redness, and discharge but rarely severe pain or swelling that spreads rapidly. Fournier’s gangrene causes intense, worsening pain, fever, tissue death, and often gas under the skin. If you’ve had yeast infections before and now feel worse than ever - don’t assume it’s the same thing.
How soon after starting SGLT2 inhibitors can Fournier’s gangrene occur?
It can happen anytime - from days to years after starting the drug. Most cases occur within the first year, but cases have been reported after 5+ years of use. There’s no safe window. Stay alert as long as you’re taking it.
Do all SGLT2 inhibitors carry this risk?
Yes. All drugs in this class - canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin - have been linked to cases. The risk appears to be a class effect, meaning it’s tied to how the drugs work, not one specific brand.
Can I get tested for Fournier’s gangrene before it happens?
No. There’s no blood test or scan that predicts it. It’s diagnosed when symptoms appear - through physical exam, imaging, and sometimes tissue biopsy. Prevention is about awareness and quick action, not screening.
What happens if I stop the drug after noticing symptoms?
Stopping the drug won’t cure the infection - but it removes the fuel for bacteria. You still need antibiotics and surgery. Stopping it is a necessary step, but not sufficient. Immediate medical care is non-negotiable.
Are there safer alternatives to SGLT2 inhibitors?
Yes. GLP-1 agonists like semaglutide (Wegovy, Ozempic) and liraglutide (Victoza) lower blood sugar and protect the heart and kidneys without increasing Fournier’s gangrene risk. DPP-4 inhibitors and metformin are other options. Talk to your doctor about switching if you’re concerned.

Glenda Marínez Granados 20.01.2026
So let me get this straight... we're giving people a drug that turns their pee into a sugar buffet for flesh-eating bacteria, and the solution is to just "know the signs"? 🤦♀️ I mean, sure, it's rare... but so is winning the lottery. And yet we don't hand out lottery tickets with a warning that says "if you win, you'll be rich but also dead." 😅
Yuri Hyuga 20.01.2026
This is one of those moments where medicine meets real life - and it’s terrifying. But here’s the beautiful part: awareness saves lives. 🌟 You don’t need to fear this drug - you need to *respect* it. Know the signs. Talk to your partner. Keep your sugars in check. And if something feels *off*? Go to the ER like your life depends on it - because it does. You’ve got this. 💪❤️
MARILYN ONEILL 20.01.2026
I mean, if you're on one of these drugs and you're not a total health nut who washes daily and checks your HbA1c like it's your job, you kinda deserve what you get. Like, why are you even on this med if you're just gonna ignore hygiene and eat cake? 😒
Coral Bosley 20.01.2026
I’ve had three yeast infections in six months since starting my SGLT2. I thought it was just bad luck. Now I’m terrified. I didn’t even know this could turn into... *that*. I’m switching tomorrow. I don’t care what my doctor says. I’m not risking my body for a pill that makes my pee sweet. I’m done. 😔
Steve Hesketh 20.01.2026
Listen, my friend - you are not alone. I’ve seen too many people dismiss these warnings because they think "it won’t happen to me." But here’s the truth: it only takes one moment of hesitation to lose everything. You’re not weak for being scared. You’re wise for paying attention. Keep your skin clean, keep your sugars low, and if you feel even a twinge of wrongness - RUN to the hospital. Your life is worth more than a delay. I believe in you. 🙏
Kevin Narvaes 20.01.2026
so like... if u got diabetes and ur pee is sugary, and u get an infection... its like... the bacteria just vibin' on the sugar? and then ur body just... melts? like in a movie? lol. i mean, why dont they just make the drug less sugary? or put a filter in the pee? 🤔
Dee Monroe 20.01.2026
I’ve been thinking about this a lot since my dad passed from a similar infection years ago - not from a drug, but from uncontrolled diabetes. There’s something haunting about how quietly these things creep up. It’s not dramatic until it’s too late. The real tragedy isn’t the drug - it’s how little we’re taught to listen to our own bodies. We’re conditioned to wait for symptoms to scream. But Fournier’s gangrene doesn’t scream - it whispers. And if you’re not trained to hear that whisper, you’ll never know it’s there until it’s already eating you alive. We need to teach people to feel their bodies like they’re sacred instruments - not machines to be managed with pills and checklists.
Alex Carletti Gouvea 20.01.2026
America’s healthcare system is a joke. You give people a drug that can kill them, then tell them to "watch for signs" like it’s a game of hide-and-seek. In my country, we just don’t prescribe this stuff unless you’re in perfect health. Why are we playing Russian roulette with people’s lives? This isn’t innovation - it’s negligence dressed up as science.
Philip Williams 20.01.2026
The data is clear: the incidence rate remains extremely low - approximately 1.9 per 100,000 patient-years. The benefits of cardiovascular and renal protection are well-documented and substantial. While the risk of Fournier’s gangrene is real, it is not a reason to abandon an evidence-based therapy for the majority of patients. Vigilance, education, and prompt intervention remain the cornerstones of safe use. Physicians should continue prescribing these agents with appropriate counseling.
Kelly McRainey Moore 20.01.2026
I’m on empagliflozin and I’ve never felt better. My A1c dropped from 8.9 to 6.2. But I do wash like a maniac now. Twice a day. No exceptions. I even bought those fancy cotton undies. If this keeps me alive, it’s worth it. Just don’t ignore the weird stuff. I learned that the hard way.
lokesh prasanth 20.01.2026
sugar in pee = bacteria party. stop the drug. go to er. done. why is this even a thing? people are so lazy they think meds are magic. nope. your body still needs to work. dumb.