Biologics Exclusivity: What It Means for Drug Prices and Access
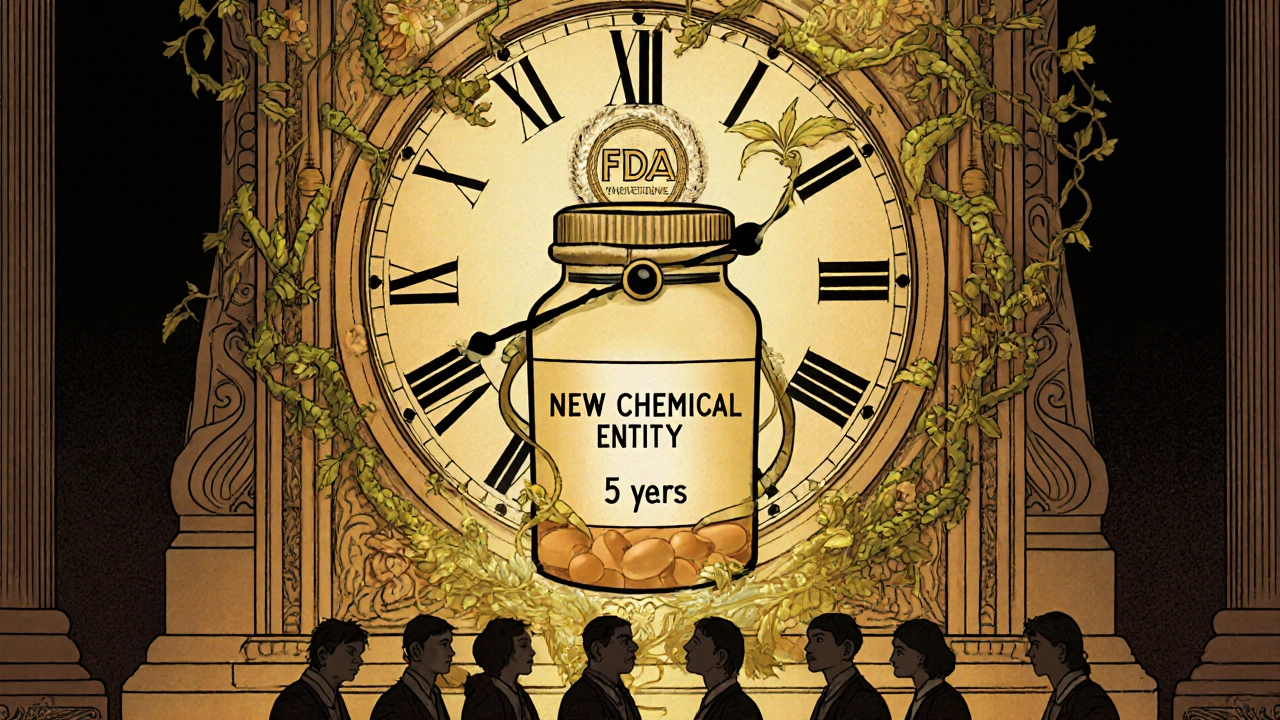
When you hear biologics exclusivity, a period of market protection granted to brand-name biologic drugs to prevent generic copies from entering the market. Also known as data exclusivity, it’s not a patent—it’s a separate legal shield that stops competitors from using the original maker’s clinical trial data to get approval for cheaper versions. This rule exists because biologics are made from living cells, not chemicals, making them far harder to copy than pills. Unlike regular drugs, you can’t just reverse-engineer a biologic. That’s why regulators require full, expensive studies to prove a copy works the same—something the original company already paid for.
That’s where biosimilars, highly similar versions of biologic drugs that are approved after exclusivity ends. Also known as follow-on biologics, they’re not exact copies, but they must show no meaningful difference in safety or effectiveness. The U.S. gives 12 years of exclusivity; Canada and the EU offer 10. During that time, no biosimilar can be approved—even if someone else develops it. This delays price drops. For example, Humira, a biologic for arthritis, had no competition for over a decade in the U.S., keeping prices near $7,000 per month. When biosimilars finally arrived, prices dropped by 30-50%, but only after years of patients paying more.
Meanwhile, drug pricing, how much patients and insurers pay for medications, often tied directly to exclusivity periods. Also known as pharmaceutical cost control, it’s the real-world impact of these rules. People with autoimmune diseases, cancer, or rare conditions often rely on biologics. If exclusivity lasts too long, they’re stuck paying high prices. Some argue the system encourages innovation. Others say it locks in profits while patients wait. The truth? Exclusivity isn’t bad by design—it’s meant to reward R&D. But when it stretches too far, it becomes a barrier to care.
You’ll find posts here that dig into how these rules affect real treatments—like why some biologics cost ten times more than their biosimilars, how long you might wait for a cheaper option, and what happens when a drug’s exclusivity ends. We break down how these protections shape what your doctor can prescribe, what your insurance covers, and why some medications stay expensive even when science says they shouldn’t. Whether you’re paying out of pocket or navigating insurance, understanding biologics exclusivity helps you ask the right questions.