Bronchodilators and Their Role in Treating Bronchitis
Learn how bronchodilators work, when they’re right for bronchitis, key types, proper inhaler use, benefits, side‑effects, and FAQs.
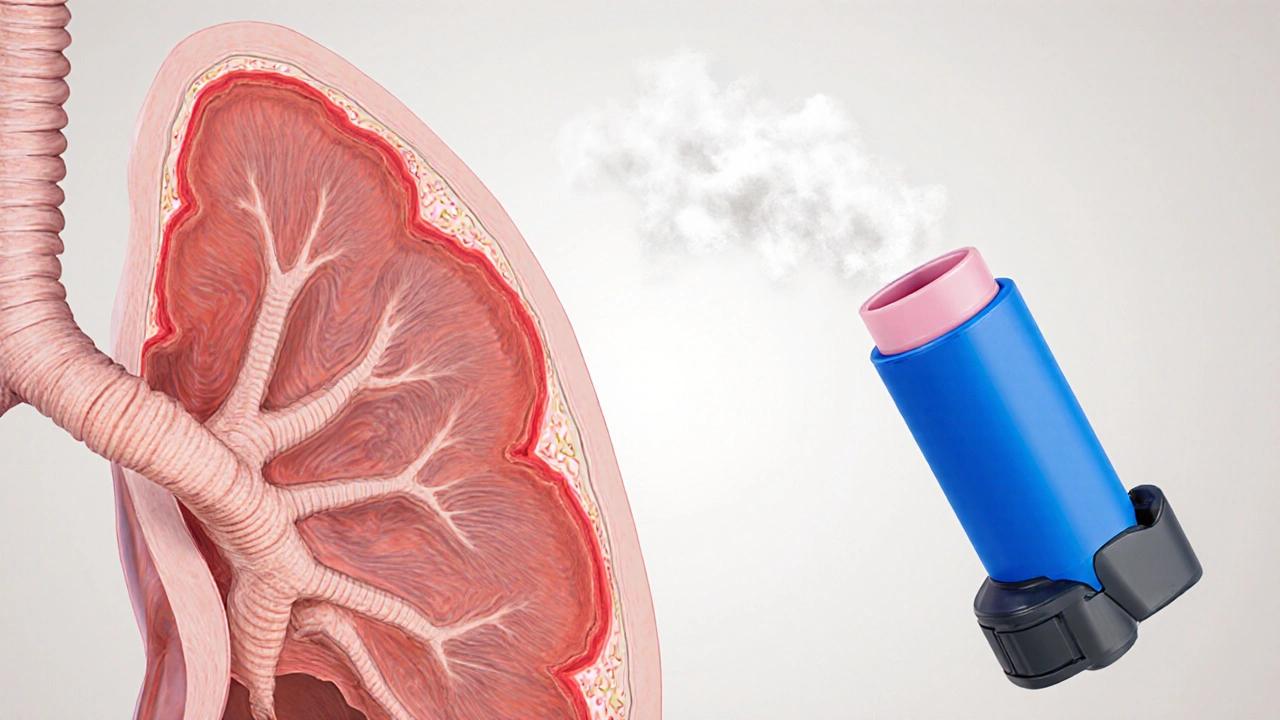
When dealing with breathing problems, understanding bronchodilators, medicines that relax the airway muscles to widen the breathing tubes. Also known as airway relaxants, they are a cornerstone of therapy for conditions that restrict airflow.
One of the most common conditions that calls for bronchodilators is asthma, a chronic inflammation of the airways that causes wheezing, coughing, and shortness of breath. Asthma episodes flare up when smooth muscles around the bronchi contract, and bronchodilators step in to reverse that contraction. Bronchodilators also play a vital role in managing COPD, a progressive lung disease that includes chronic bronchitis and emphysema, where airflow limitation is more permanent but still benefits from occasional muscle relaxation.
Bronchodilators rarely work in isolation. They are most effective when paired with inhaled corticosteroids, anti‑inflammatory drugs that reduce swelling in the airway walls. The combination addresses both the muscle tightening and the underlying inflammation, giving patients better symptom control. Another frequent partner is the beta‑agonist, a class of bronchodilators that stimulate beta‑2 receptors to cause rapid muscle relaxation. Short‑acting beta‑agonists (SABAs) act fast for attacks, while long‑acting beta‑agonists (LABAs) provide steady relief throughout the day.
Choosing the right bronchodilator involves matching its pharmacologic profile to the patient’s needs. Short‑acting agents are ideal for rescue use because they work within minutes, but they shouldn’t replace daily maintenance therapy. Long‑acting agents, meanwhile, need a prescription and are usually taken twice daily; they are often combined with inhaled corticosteroids in a single inhaler for convenience. Understanding these nuances helps readers avoid common pitfalls like over‑reliance on rescue inhalers or missing daily anti‑inflammatory doses.
Beyond the drugs themselves, delivery devices matter. Metered‑dose inhalers, dry‑powder inhalers, and nebulizers each have pros and cons related to dose accuracy, ease of use, and portability. Patients who struggle with hand‑lung coordination may benefit from a spacer or a breath‑actuated device. Recognizing how device choice interacts with medication type provides a more complete picture of effective breathing support.
The articles below dive deeper into each of these topics—whether you’re comparing specific bronchodilator brands, learning how inhaled corticosteroids boost your regimen, or figuring out which device fits your lifestyle. Browse the collection to find practical tips, side‑effect warnings, and real‑world comparisons that will help you make informed decisions about your respiratory health.
Learn how bronchodilators work, when they’re right for bronchitis, key types, proper inhaler use, benefits, side‑effects, and FAQs.