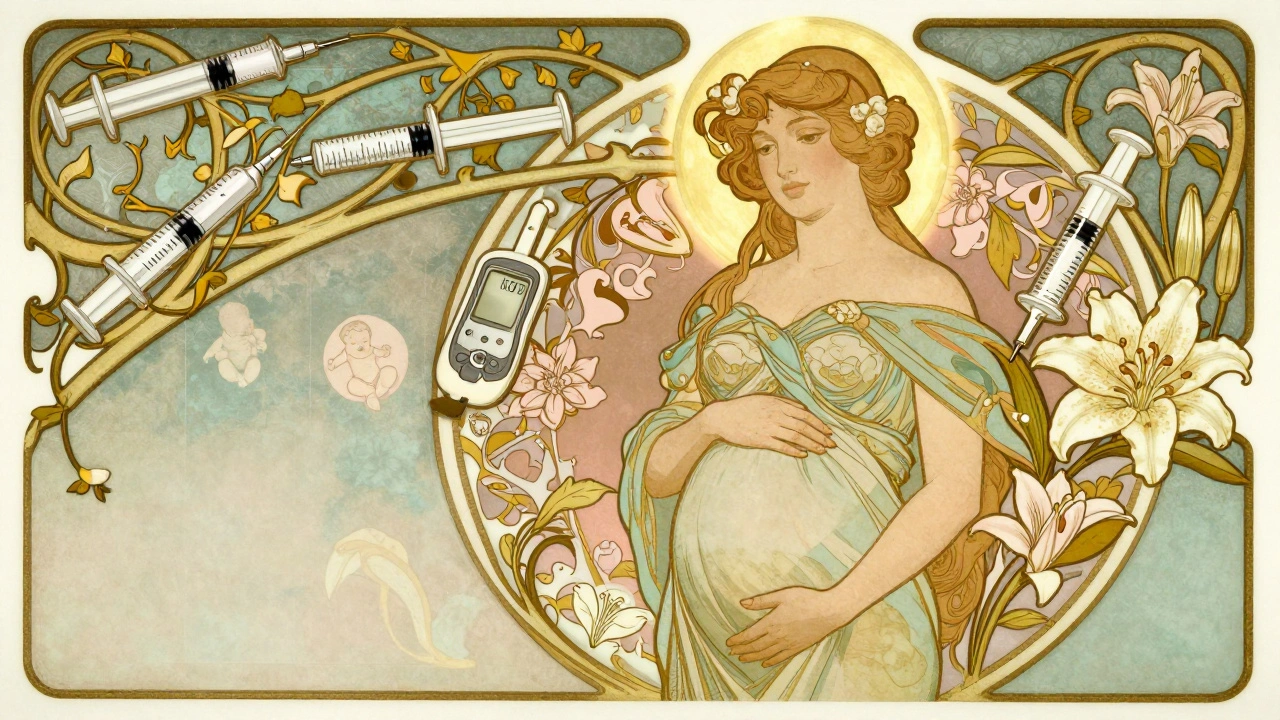
Diabetes During Pregnancy: Risks, Management, and What You Need to Know
When diabetes during pregnancy, a condition where blood sugar levels rise during gestation, often for the first time. Also known as gestational diabetes, it affects about 6 to 9% of pregnant women in the U.S. and doesn’t mean you had diabetes before—you just can’t process sugar the way your body used to. This isn’t just a temporary glitch. Left unmanaged, it can lead to complications like preterm birth, large baby size, and even future type 2 diabetes for both mother and child.
What makes gestational diabetes, a form of insulin resistance triggered by pregnancy hormones so tricky is that symptoms are often silent. You might feel fine, but your pancreas is struggling to keep up with the extra demand. That’s why routine screening between 24 and 28 weeks matters. Even if you’ve never had high blood sugar before, your body changes during pregnancy in ways that can push you over the edge. blood sugar control, the daily practice of monitoring and managing glucose levels through diet, movement, and sometimes medication becomes your new normal. It’s not about perfection—it’s about consistency. Eating balanced meals, walking after meals, and checking your levels as advised can make all the difference.
Some women manage with diet and exercise alone. Others need pregnancy and insulin, a safe, non-oral treatment option that doesn’t cross the placenta and is commonly used when lifestyle changes aren’t enough. Insulin isn’t a failure—it’s a tool. Many women worry about shots, but modern pens are tiny, nearly painless, and far safer than letting blood sugar run high. Oral meds like metformin are sometimes used off-label, but insulin remains the gold standard when you need more control.
After delivery, most women’s blood sugar returns to normal—but the risk doesn’t vanish. Up to half of women with gestational diabetes develop type 2 diabetes within 10 years. That’s why follow-up testing at 6 to 12 weeks postpartum is critical. And if you plan to have another child, knowing your history helps your doctor prepare early. This isn’t just about one pregnancy. It’s about your long-term health.
You’ll find real stories here—not theory. Posts cover how to handle low blood sugar at 3 a.m., what foods actually help stabilize glucose, why some women need insulin while others don’t, and how to talk to your provider when you feel overwhelmed. You’ll also learn about the hidden risks, like preeclampsia and neonatal hypoglycemia, and how to spot them before they become emergencies. No fluff. No guesswork. Just what works, what to avoid, and how to take back control during a time when your body feels like it’s working against you.