Gestational Diabetes Meds: Safe Options, Risks, and What Your Doctor Wants You to Know
When you're pregnant and diagnosed with gestational diabetes, a type of diabetes that develops during pregnancy due to hormonal changes affecting insulin sensitivity. It's not your fault, and it's not permanent—but it needs careful management to protect both you and your baby. About 6-9% of pregnant people in North America get it, and while diet and exercise often help, sometimes you need medication, a treatment used to control blood sugar when lifestyle changes aren't enough to keep things on track.
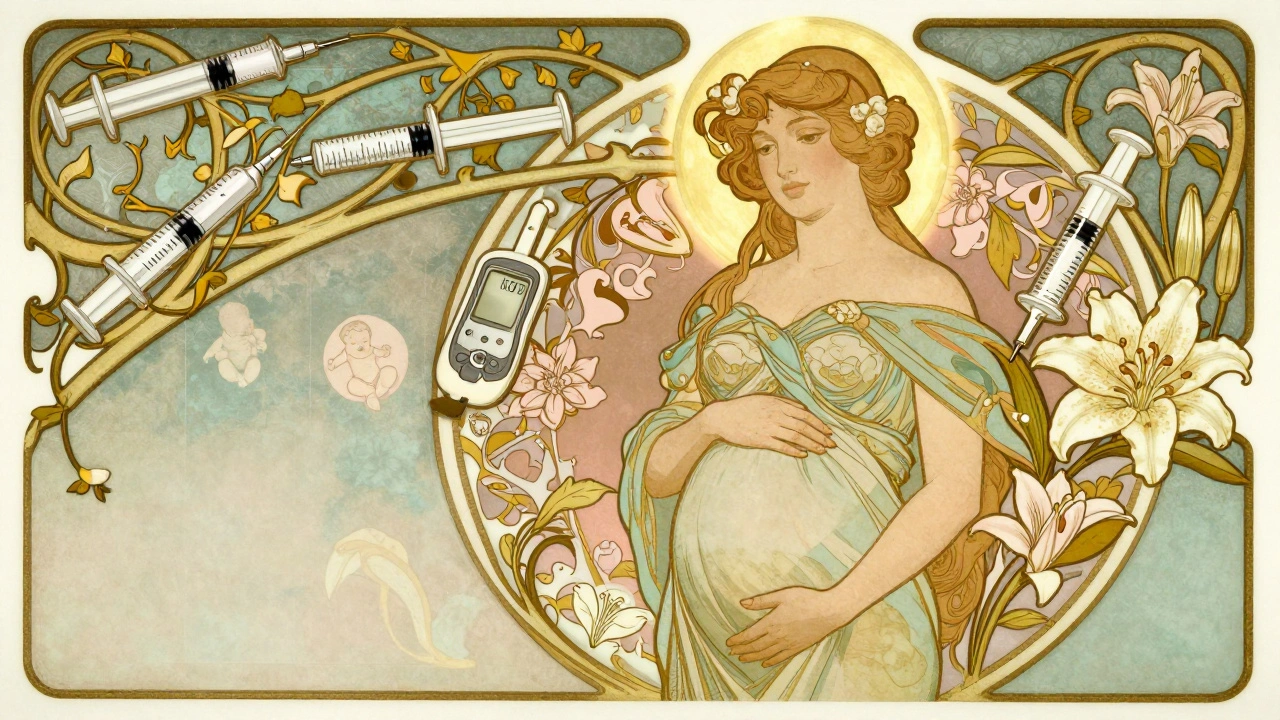
The two main gestational diabetes meds, prescription drugs approved for use during pregnancy to lower high blood sugar are insulin and metformin. Insulin is the gold standard—it doesn’t cross the placenta, so it won’t affect the baby directly. Many doctors start here because it’s been used safely for decades. Metformin, an oral pill, is becoming more common. It crosses the placenta, but studies show no increased risk of birth defects or long-term harm. Some women prefer it because it’s easier than shots, but not everyone responds well. Your doctor will pick based on your blood sugar levels, weight, and how your body reacts.
Other drugs like sulfonylureas (e.g., glyburide) are sometimes used off-label, but they carry more risk of low blood sugar in the baby and are less preferred now. What you won’t see? GLP-1 agonists or SGLT2 inhibitors—they’re not approved for pregnancy. And no, you don’t need to panic if you’ve been taking metformin before pregnancy; many continue it under supervision. The goal isn’t to eliminate sugar completely—it’s to keep your levels steady so your baby doesn’t grow too large, avoid preterm labor, and reduce your chance of needing a C-section.
Monitoring matters just as much as meds. You’ll likely check your blood sugar four times a day—at fasting and after meals. If your numbers stay high despite meds, your doctor might adjust your dose or switch treatments. Some women only need meds for a few weeks. Others need them until delivery. And yes, most gestational diabetes goes away after birth—but you’re at higher risk for type 2 diabetes later, so follow-up testing is key.
What you won’t find in this collection? Fluff about miracle diets or supplements that claim to cure it. Instead, you’ll get real talk about what works, what doesn’t, and what the science actually says. You’ll see how gestational diabetes meds interact with other pregnancy meds, what side effects to watch for, and why some women end up on insulin even if they swore they’d avoid it. You’ll also find posts on how to talk to your doctor about options, what to do if you miss a dose, and how to manage blood sugar spikes after eating. This isn’t theory—it’s what people are actually using, struggling with, and surviving.