Bronchodilators and Their Role in Treating Bronchitis
Learn how bronchodilators work, when they’re right for bronchitis, key types, proper inhaler use, benefits, side‑effects, and FAQs.
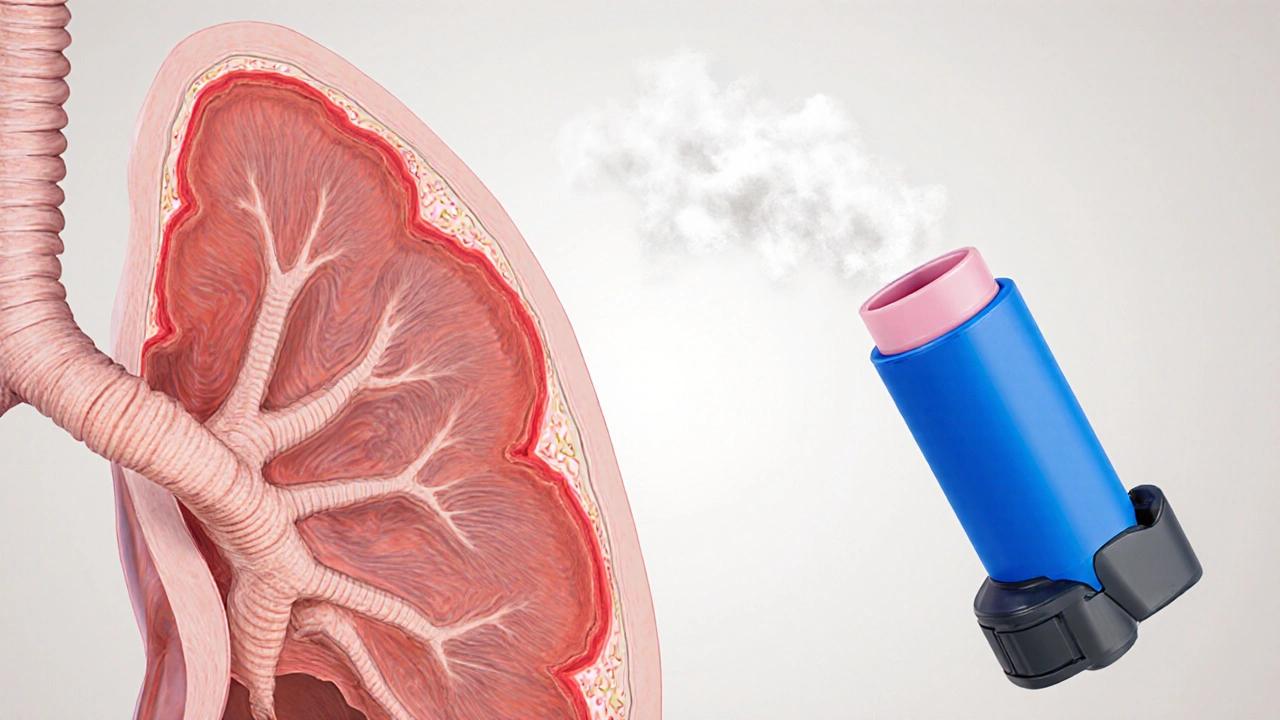
When talking about inhaler therapy, the use of portable devices to deliver medication directly into the lungs for respiratory conditions. Also known as inhalation treatment, it serves as the backbone of modern asthma and COPD management. Alongside it, Inhaled Corticosteroids, anti‑inflammatory drugs that reduce airway swelling and prevent attacks are the most common class of drugs. The delivery vehicles matter too: the Metered‑Dose Inhaler (MDI), a press‑urized canister that sprays a fine mist when you press the mouthpiece and the Nebulizer, a machine that turns liquid medication into an aerosol you breathe through a mask or mouthpiece are the two giants in the field. Together they form a three‑part system: drug, device, and patient technique, each influencing how well the medication reaches the lower airways.
Inhaler therapy encompasses a range of devices, from dry‑powder inhalers that rely on the patient’s own breath power to soft‑mist inhalers that generate a slower, longer‑lasting plume. It requires proper inhalation technique—slow, deep breaths for dry‑powder devices, coordinated actuation‑inhalation for MDIs, and steady tidal breathing for nebulizers. The choice of device often hinges on the underlying condition: Asthma, a chronic inflammatory disease characterized by reversible airway narrowing typically responds well to MDIs paired with quick‑relief bronchodilators, while Chronic Obstructive Pulmonary Disease (COPD), a progressive blockage of airflow that isn’t fully reversible may need higher‑dose inhaled steroids delivered via nebulizer for better deposition. Bronchodilators, medications that relax airway muscles for immediate symptom relief often accompany inhaled steroids, forming a dual‑therapy strategy that tackles both inflammation and constriction. Understanding how each device’s particle size, velocity, and humidification affect drug placement helps clinicians match the right tool to the patient’s age, dexterity, and disease severity.
Beyond the devices themselves, inhaler therapy interacts with broader care plans—regular lung function monitoring, trigger avoidance, and patient education. For children, spacers attached to MDIs can reduce coordination demands, while older adults may prefer nebulizers that eliminate the need to time breaths. Side‑effects such as oral thrush from inhaled steroids or throat irritation from bronchodilators can be mitigated with simple steps like rinsing the mouth after each use. Insurance coverage, cost, and availability also shape which device becomes the default option in a given setting. As new formulations emerge, like ultra‑low‑dose corticosteroid sprays or combination inhalers that bundle steroids and bronchodilators, the therapeutic landscape keeps evolving, demanding that patients stay informed and clinicians stay agile.
Below you’ll find a curated set of articles that break down these concepts in plain language. From head‑to‑head comparisons of inhaled steroids to step‑by‑step guides on mastering MDI technique, the collection covers everything a newcomer or seasoned user needs to make the most of inhaler therapy. Dive in to discover which device fits your lifestyle, how to avoid common pitfalls, and what the latest research says about optimal dosing.
Learn how bronchodilators work, when they’re right for bronchitis, key types, proper inhaler use, benefits, side‑effects, and FAQs.