Oral Diabetes Drugs and Pregnancy: What You Need to Know
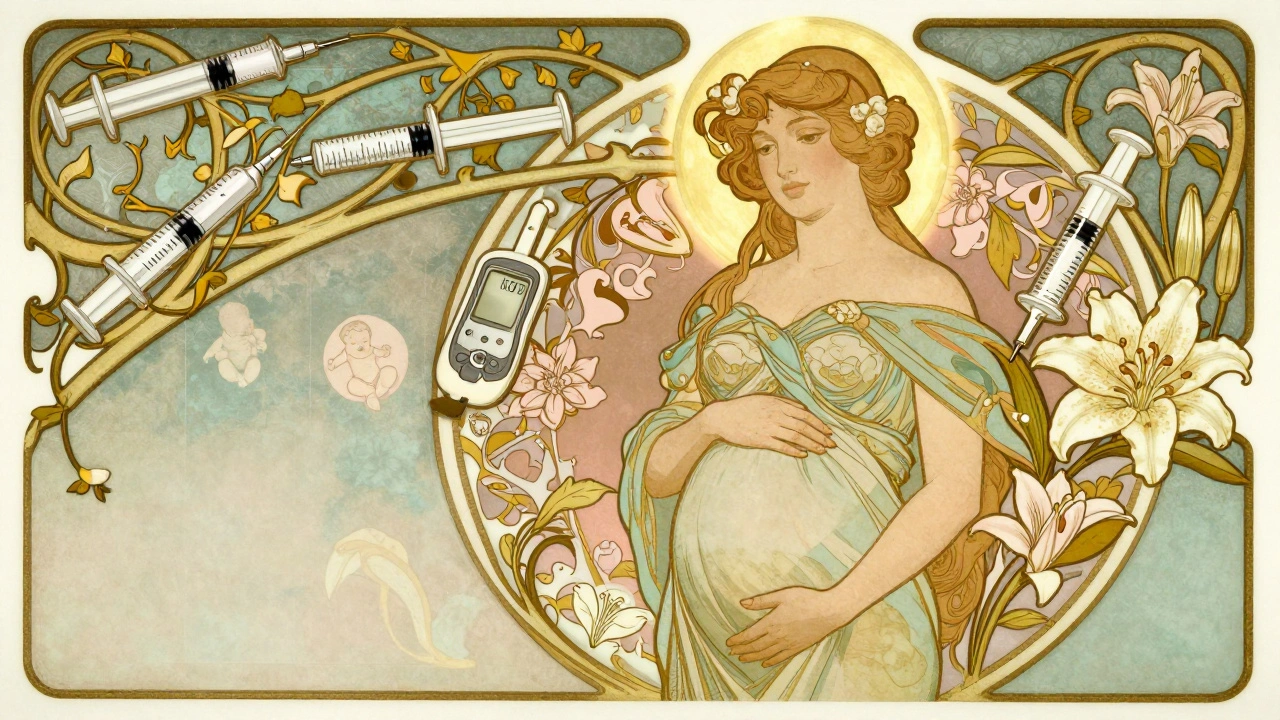
When you have oral diabetes drugs, medications taken by mouth to manage blood sugar in type 2 diabetes or gestational diabetes, and find out you’re pregnant, it’s normal to panic. You’re not just thinking about your health anymore—you’re thinking about your baby. The big question isn’t just "Can I keep taking my pill?" It’s "Will it hurt my child?" The truth is, some oral diabetes drugs are used safely during pregnancy, while others are avoided. metformin, a common first-line oral drug for type 2 diabetes that crosses the placenta but has years of safety data in pregnancy is often continued, especially if insulin isn’t an option. insulin, the gold standard for blood sugar control in pregnancy because it doesn’t cross the placenta is preferred in many cases, but not everyone can or wants to use injections.
Doctors don’t make these choices lightly. They weigh what’s known from real-world use—not just lab studies. For example, metformin has been tracked in thousands of pregnancies, and no major birth defects have been linked to it. Sulfonylureas like glyburide are sometimes used, especially in gestational diabetes, but they carry a higher risk of low blood sugar in the baby after birth. That’s why many providers avoid them unless absolutely necessary. The goal isn’t to stop all medication—it’s to keep your blood sugar in a tight, safe range. High blood sugar during pregnancy increases risks like preterm birth, large babies, and even stillbirth. That’s why even if you’re nervous about pills, letting your sugar run high is often riskier.
What you won’t find in most guides is how messy this decision really is. Some women switch to insulin before conception. Others stay on metformin until their OB says otherwise. A few stop cold and try diet and exercise first. There’s no one-size-fits-all plan. What matters is working with a team—your OB, endocrinologist, and pharmacist—who understand both diabetes and pregnancy. You need to know what your pills do, what alternatives exist, and how to spot warning signs like dizziness, extreme thirst, or blurry vision. The posts below cover real cases, drug interactions to watch for, and how to talk to your doctor without feeling rushed or dismissed. You’ll find practical advice on managing blood sugar without insulin, what to expect during prenatal visits, and how to spot when a medication might be doing more harm than good. This isn’t theory. It’s what real women and their doctors are dealing with right now.