Warfarin Antibiotic Risk Calculator
This calculator estimates your risk of dangerous INR spikes when taking certain antibiotics with warfarin. Based on your answers, it will provide personalized recommendations to prevent bleeding complications.
Your Risk Factors
When you’re on warfarin, even a simple antibiotic can turn dangerous. Trimethoprim-sulfamethoxazole - sold under brand names like Bactrim or Septra - is one of the most common antibiotics prescribed for urinary tract infections, sinus infections, and bronchitis. But if you’re taking warfarin to prevent strokes, clots, or manage a mechanical heart valve, this combo can send your INR soaring - sometimes to life-threatening levels.
What Happens When These Two Drugs Meet?
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a tightrope walk: too little, and you risk clots; too much, and you bleed. Your INR tells you where you stand. A normal therapeutic range is usually 2.0 to 3.0. But when you start trimethoprim-sulfamethoxazole, that number can jump by 1.5 to 2.5 points within just 36 to 72 hours. This isn’t random. The interaction has three clear mechanisms. First, trimethoprim blocks the CYP2C9 enzyme - the same one your liver uses to break down the most powerful form of warfarin, called S-warfarin. When this enzyme slows down, warfarin builds up in your blood. Second, sulfamethoxazole pushes warfarin off protein binding sites in your bloodstream. Since warfarin is 97% bound to albumin, even a small displacement can significantly increase the active drug floating around. Third, the antibiotic wipes out gut bacteria that produce vitamin K. Less vitamin K means warfarin works even harder. The result? A sudden, unpredictable rise in INR. Studies show TMP-SMX raises INR by an average of 1.8 units. Compare that to amoxicillin, which barely moves the needle - just 0.4 units. Fluoroquinolones like ciprofloxacin are in the middle. But TMP-SMX? It’s the worst offender among common antibiotics.Who’s at Highest Risk?
Not everyone reacts the same way. Some people take Bactrim and their INR barely budges. Others go from 2.5 to 7.0 in three days. Why? Age matters. People over 75 are far more likely to see big INR spikes. Liver problems? That’s another red flag. Your liver handles warfarin metabolism - if it’s not working well, the drug lingers. Poor nutrition, especially low vitamin K intake from leafy greens, makes things worse. And men? They’re 9% more likely than women to have a dangerous reaction, according to a study of over 70,000 patients. If you have a mechanical heart valve, you’re already in the danger zone. Your target INR is usually 2.5 to 3.5 - right in the range where even a small bump can trigger bleeding. One case reported in a medical forum involved a 78-year-old man with a mechanical aortic valve. His INR hit 8.2 after three days of TMP-SMX. He needed vitamin K and fresh frozen plasma to stabilize.Real Stories, Real Consequences
Behind the numbers are real people. A nurse practitioner on an anticoagulation forum described multiple elderly patients whose INR jumped from 2.5 to 6.0 after starting Bactrim for a UTI. One ended up in the ER with a subdural hematoma. Another had gastrointestinal bleeding that required a blood transfusion. FDA data shows over 1,800 reports of INR elevation linked to TMP-SMX in just five years. Nearly half led to hospitalization. And 68 of those cases ended in death from bleeding. But it’s not always catastrophic. Some patients - especially younger, healthier ones with stable INRs - tolerate the combo without issue. A pharmacist on Reddit shared a case where a 62-year-old man took TMP-SMX for pneumonia for seven days. His INR stayed at 2.8. He was lucky. But luck isn’t a strategy.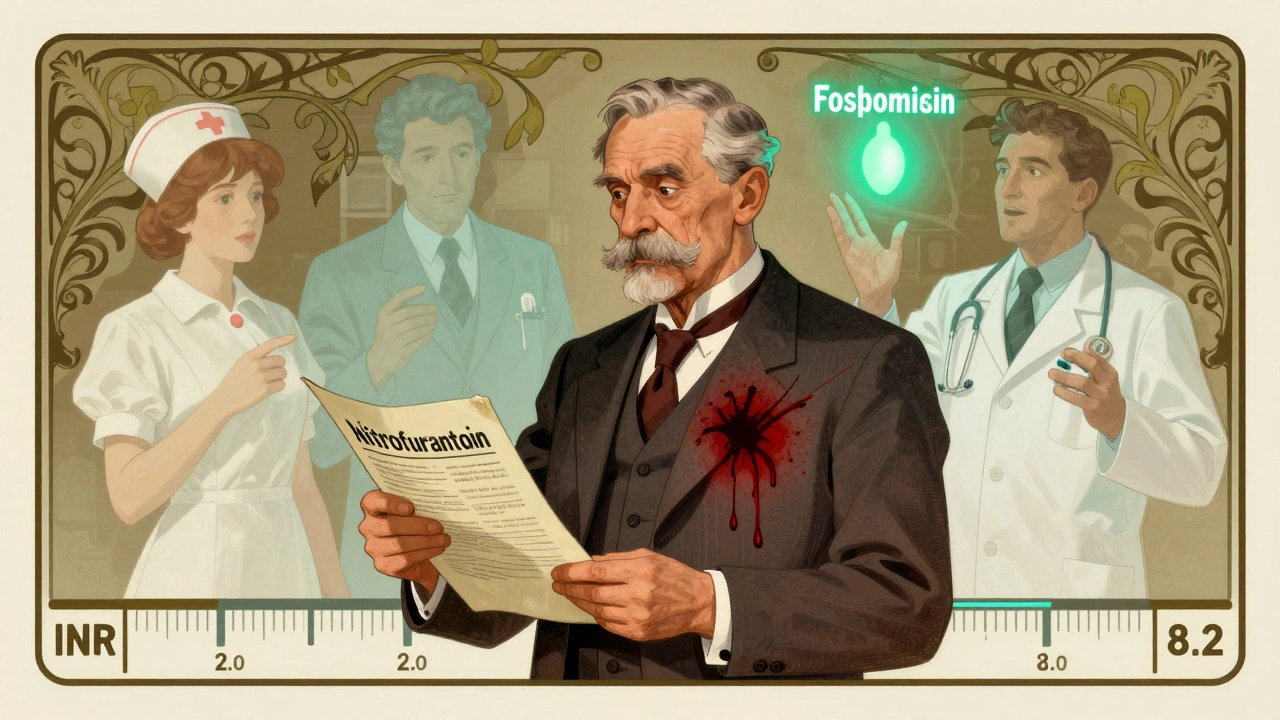
What Doctors Should Do - And What You Should Ask
Expert guidelines are clear: avoid TMP-SMX if you’re on warfarin. Period. The American Heart Association and the American College of Chest Physicians both say: use alternatives. For urinary tract infections, nitrofurantoin or fosfomycin are safer. For sinus infections, amoxicillin or doxycycline usually work. But sometimes, there’s no choice. If you have a severe infection and no other antibiotic will do, here’s what needs to happen:- Check your INR before starting TMP-SMX.
- Reduce your warfarin dose by 20-30% on day one - especially if you’re over 70 or have liver issues.
- Test your INR again within 48 hours. Don’t wait. Don’t assume it’s fine.
- Check again every 3-4 days while on the antibiotic.
What You Can Do Right Now
If you’re on warfarin and your doctor prescribes TMP-SMX, ask: Is there a safer antibiotic? Don’t accept “it’s just a little Bactrim.” That phrase has landed people in the hospital. Keep a log. Write down your INR numbers, your warfarin dose, and any new medications - even over-the-counter ones. Bring it to every appointment. Many bleeding events happen because patients don’t tell their providers about new prescriptions. Educate yourself. The National Blood Clot Alliance found that patients who got specific counseling about antibiotic interactions had 37% fewer emergency visits for bleeding. That’s not minor. That’s life-saving.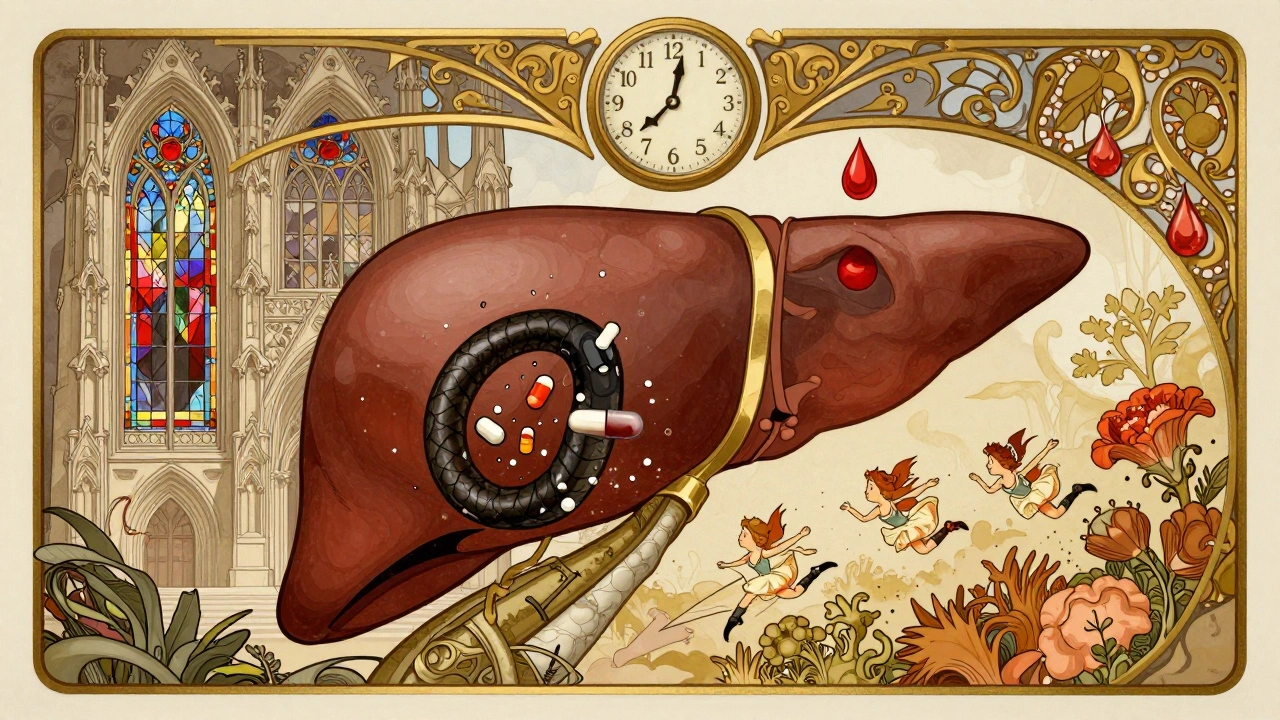
The Bigger Picture
Even though newer blood thinners like apixaban and rivaroxaban are replacing warfarin for many people, over 2.6 million Americans still take it in 2025. And TMP-SMX remains one of the top 50 prescribed antibiotics. That means this interaction isn’t going away. New research is trying to predict who’s at risk. A 2023 study created an algorithm using CYP2C9 and VKORC1 genes, age, and baseline INR. It predicted dangerous spikes with 82% accuracy. That’s promising. But we’re not there yet. For now, the safest rule is simple: avoid TMP-SMX if you’re on warfarin. Always.What to Do If Your INR Spikes
If you notice unusual bruising, bleeding gums, blood in urine or stool, or sudden headaches, don’t wait. Call your anticoagulation clinic or go to the ER. Time matters. INR above 5.0 with bleeding needs immediate action. Don’t delay because you think it’s “just a little bleeding.” Warfarin doesn’t play fair.Can I take Bactrim if I’m on warfarin?
Avoid it if possible. TMP-SMX (Bactrim) significantly increases the risk of dangerous INR spikes and bleeding. Safer antibiotics like nitrofurantoin or amoxicillin are usually available. Only use Bactrim if no alternatives exist, and only under close INR monitoring.
How quickly does INR rise after starting TMP-SMX?
INR typically starts rising within 36 to 72 hours after starting TMP-SMX. That’s why checking your INR within 48 hours is critical - waiting longer risks missing a dangerous spike.
What’s the safest antibiotic for someone on warfarin?
For urinary tract infections, nitrofurantoin or fosfomycin are preferred. For respiratory infections, amoxicillin, doxycycline, or azithromycin are generally safe. Always confirm with your provider - not all antibiotics are equal.
Should I stop warfarin if I need Bactrim?
Never stop warfarin on your own. Instead, reduce your dose by 20-30% before starting Bactrim and check your INR within 48 hours. Stopping warfarin suddenly can cause clots. Adjusting the dose under medical supervision is the right approach.
Can I eat leafy greens while on warfarin and Bactrim?
Yes - but keep your intake consistent. Sudden changes in vitamin K-rich foods (like spinach, kale, broccoli) can affect INR. Bactrim reduces vitamin K from gut bacteria, so maintaining steady dietary intake helps avoid extra fluctuations.
How often should INR be checked during TMP-SMX therapy?
Check INR before starting, then again at 48-72 hours. After that, check every 3-4 days while on the antibiotic. Once you stop Bactrim, continue checking every 2-3 days for a week, as INR may drop suddenly.
Are newer blood thinners safer with antibiotics?
Yes. DOACs like apixaban, rivaroxaban, and dabigatran have far fewer antibiotic interactions than warfarin. TMP-SMX doesn’t significantly affect their levels. If you’re on warfarin and frequently need antibiotics, talk to your doctor about switching - especially if you’re over 65 or have unstable INRs.


Annie Grajewski 4.12.2025
so like... i took bactrim last year for a uti and my inr went to 6.8 and i ended up in the er with a nosebleed that wouldn't stop. my dr just shrugged and said 'oops, sorry' and gave me vitamin k. no follow up. no warning. just... 'here's your script' like it's a damn candy bar. why do doctors not tell you this stuff before you're bleeding out??
Mark Ziegenbein 4.12.2025
Let me be clear: this isn't merely a pharmacokinetic interaction-it's a systemic failure of medical education. The CYP2C9 enzyme isn't some obscure biochemical curiosity; it's the very gatekeeper of warfarin metabolism, and when trimethoprim slams that door shut while sulfamethoxazole kicks the albumin-bound warfarin into circulation like a drunken bouncer at a club, you're not just 'at risk'-you're playing Russian roulette with your cerebral vasculature. And yet, we still prescribe this combo like it's tea and crumpets. The real tragedy? It's entirely preventable. But prevention requires humility, and humility is in short supply in modern medicine.
Norene Fulwiler 4.12.2025
I've worked in anticoagulation clinics for 14 years. I've seen patients lose limbs because they were told 'it's just a little Bactrim.' One woman, 79, had a GI bleed after her grandson's pediatrician prescribed it for her sinus infection-she didn't even know she was on warfarin. We need better communication-not just between doctors and patients, but between specialties. Pharmacists should be flagged automatically when warfarin and TMP-SMX are prescribed together. It's not rocket science. It's basic safety.
William Chin 4.12.2025
As a licensed clinical pharmacist with board certification in anticoagulation therapy, I must emphasize that the data presented here is not merely anecdotal-it is evidence-based, peer-reviewed, and supported by multiple meta-analyses including those published in the Journal of Thrombosis and Haemostasis and the American Journal of Health-System Pharmacy. The 1.8-unit INR elevation is statistically significant (p < 0.001), and the risk of major hemorrhage increases exponentially above an INR of 5.0. Therefore, it is imperative that all prescribers adhere to the ACCP and AHA guidelines without exception. Failure to do so constitutes a deviation from the standard of care.
James Moore 4.12.2025
Look, I don't care what your 'expert guidelines' say-America is being turned into a nation of cowards who can't even take an antibiotic without a 12-page consent form. My grandfather took Bactrim for 10 years with warfarin and lived to 92. He never bled. He never went to the hospital. He smoked, drank, ate bacon, and still walked his dog every morning. Meanwhile, we're treating 70-year-olds like fragile glass figurines because some PhD in a lab coat ran a study on 70,000 people and decided that 'risk' is a synonym for 'death.' Wake up. We're not in Sweden. We don't need to be coddled. If you're on warfarin, check your INR. If you're not, stop being a hypochondriac.
Kylee Gregory 4.12.2025
I think the real issue here isn't just the drug interaction-it's how disconnected we've become from the human side of medicine. We have all these numbers, algorithms, and guidelines, but we forget that behind every INR is someone's fear, someone's family, someone's exhaustion from having to remember a dozen meds and dietary restrictions. Maybe the solution isn't just avoiding Bactrim... but building systems that actually listen. Like pharmacists calling patients directly. Like EHRs that scream when warfarin and TMP-SMX are paired. We know what to do. We just need to care enough to do it.
Laura Saye 4.12.2025
The pharmacodynamic synergy between trimethoprim-sulfamethoxazole and warfarin is a textbook example of multi-mechanistic potentiation-CYP2C9 inhibition, protein-binding displacement, and gut microbiota depletion collectively amplify anticoagulant effect. But beyond the biochemistry, there's a profound ethical dimension: the burden of vigilance falls disproportionately on patients who are often elderly, cognitively frail, or socioeconomically marginalized. The system should bear this burden-not the individual. A simple, automated pharmacy alert with a mandatory clinical decision support pop-up could prevent 80% of these events. We have the technology. Do we have the will?
luke newton 4.12.2025
People like you think you're so smart because you read a medical article. But you don't know what real suffering is. My cousin died from a brain bleed because some doctor thought 'Bactrim was fine.' And now you're sitting here with your fancy INR numbers like it's a game. That's not medicine. That's arrogance wrapped in a white coat. You don't get to lecture people about safety when your kind is the reason people die.
Ali Bradshaw 4.12.2025
Hey, I'm a nurse in the UK and I see this all the time. We don't even prescribe Bactrim to anyone on warfarin here-it's just not done. We have alternatives, and we use them. It's not about fear, it's about responsibility. I wish more US docs took that approach. You don't need to be a genius to know that if something's labeled 'high risk' in 10 different studies, you probably shouldn't use it. Simple.
aditya dixit 4.12.2025
As someone from India where antibiotics are sold over the counter without prescription, I can say this: the real problem isn't just the interaction-it's the lack of regulation. In the U.S., at least you have guidelines. In my country, people take Bactrim for fever, cough, or just because their neighbor said it 'worked.' No INR checks. No warfarin monitoring. Just hope. I’ve seen patients collapse from bleeding after taking it for a cold. This isn't just an American issue-it's a global health crisis disguised as a drug interaction.
Lynette Myles 4.12.2025
They’re not warning you because they want you to bleed. It’s all part of the pharmaceutical control grid. Warfarin is cheap. DOACs? Expensive. Bactrim? Profitable. They don’t care if you die-they care if your insurance pays.