Getting the right dose of liquid medicine isn’t just important-it can mean the difference between recovery and hospitalization. In homes and hospitals alike, wrong-dose errors with liquid medications are one of the most common and dangerous types of medication mistakes. A 2023 study in the Journal of Pediatrics found that 80% of pediatric home medication errors involve incorrect liquid doses. That’s not a small risk. It’s a widespread, preventable problem.
Why Liquid Medications Are So Risky
Liquid medicines are tricky because they’re measured in tiny amounts. A child might need 2.5 mL of antibiotics. An adult might need 10 mL of pain relief. But most people don’t have a clear sense of what those numbers mean. A teaspoon? A tablespoon? A capful? Those aren’t precise. And that’s the problem. The Institute for Safe Medication Practices says that using non-metric units like teaspoons and tablespoons causes 28% of preventable pediatric errors every year. Even worse, many caregivers use kitchen spoons-because they’re handy. But a regular kitchen teaspoon can hold anywhere from 2.5 mL to 7 mL. That’s a 180% variation in dose. One spoon might give half the medicine needed. Another might give double-and that’s dangerous. Packaging doesn’t help. Many bottles look almost identical. Labels are small. Units get mixed up. Some still say “teaspoon” even though the FDA has warned against it since 2010. And when a pharmacist hands you a dosing cup with blurry markings? You’re already starting behind the line.The Best Tool: Oral Syringes
If you’re giving liquid medicine to a child-or even an adult who has trouble swallowing pills-use an oral syringe. Not a cup. Not a spoon. A syringe. Studies show oral syringes are 37% more accurate than dosing cups. For doses under 1 mL, syringes with 0.1 mL markings reduce error rates to just 8.2%. Dosing cups? They’re wrong 41.1% of the time for those same small doses. That’s more than 4 in 10 doses being off. The American Academy of Pediatrics has said since 2015: “Always use a syringe, not a cup.” The American Academy of Family Physicians reinforced that in 2020. And the NIH found that syringes are 94% accurate for a 2.5 mL dose. Dosing cups? Only 76%. Household spoons? Just 62%. You don’t need a fancy syringe. A simple plastic one, with clear mL markings, costs less than $1. Pharmacies should give you one with every liquid prescription. If they don’t? Ask. Politely but firmly. You’re not being difficult-you’re protecting your child’s health.Always Use Milliliters (mL)
Never, ever accept a prescription written in “teaspoons” or “tablespoons.” Demand it in milliliters (mL). The World Health Organization calls this the single most effective step to prevent errors. Why? Because people don’t know how much a teaspoon holds. But everyone understands “5 mL.” It’s exact. It’s universal. It’s safe. In 2024, the FDA moved to require all over-the-counter liquid medicines to include enclosed dosing devices with metric-only labeling. That’s progress. But it’s not universal yet. You still need to be your own advocate. When you pick up a prescription, check the label. Does it say “give 5 mL”? Good. Does it say “give 1 tsp”? That’s a red flag. Call the pharmacy. Ask them to re-label it in mL. If they refuse? Go elsewhere. There are pharmacies that get it right.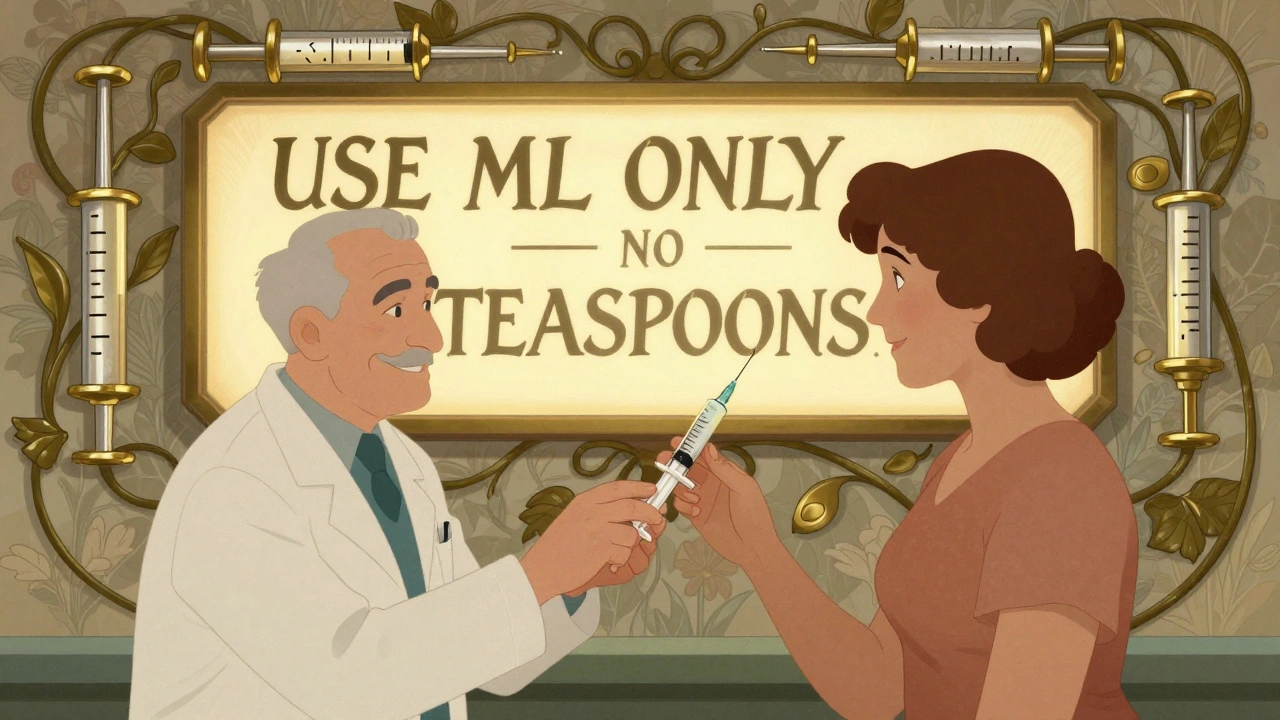
What Hospitals and Pharmacies Should Be Doing
In healthcare settings, the tools are there-but adoption is uneven. ENFit connectors are now the global standard for enteral (tube) feeding systems. Since 2016, ISO 80369-3 requires these connectors to be geometrically incompatible with IV lines. That means a feeding tube can’t accidentally plug into a vein. This prevents deadly wrong-route errors. Hospitals that switched to ENFit saw a 98% drop in these mistakes. But only 42% of U.S. hospitals have fully adopted ENFit. Why? Cost. Training. Resistance. The average hospital spends $85,000 to switch systems. That’s a lot. But the cost of one wrong-route error-death, lawsuits, lost trust-is far higher. Electronic health records (EHRs) with built-in dose-checking tools cut errors by 58%. If a doctor tries to prescribe 15 mL of a drug that should be 5 mL for a 10-pound child, the system should flag it. But only 68% of pediatric units have this feature. Adult units? Just 32%. Barcoding systems (BCMA) that scan both the patient’s wristband and the medication reduce wrong-dose errors by 48%. But they only work if staff use them every single time. Miss one scan? The safety net disappears.What You Can Do at Home
You don’t need a hospital budget to keep your family safe. Here’s your checklist:- Always use an oral syringe. Get one from the pharmacy. If they don’t give it to you, ask. Buy one online for under $2 if needed.
- Never use kitchen spoons. They’re not accurate. Period.
- Measure in mL only. If the label says “teaspoon,” call the pharmacy and ask for a corrected label.
- Store syringes with the medicine. Keep them in the same place. Don’t let them get lost or mixed up with other items.
- Double-check the dose. Read the label. Read the syringe. Read it again. Ask a second person to confirm if you’re unsure.
- Take a photo of the prescription. If you’re ever confused later, you’ll have a record of what was ordered.
- Ask for pre-measured doses. Some pharmacies offer dose packs-syringes already filled with the exact amount. These are ideal for busy parents or elderly patients. Satisfaction rates? 94%.
Common Mistakes and How to Avoid Them
Here are the top mistakes caregivers make-and how to stop them:- Mistake: “I gave the last dose, so I’ll just guess this one.” Solution: Always measure. Even if it’s the same medicine.
- Mistake: “The cup looked close enough.” Solution: Cups are the #1 cause of overdoses. Use a syringe.
- Mistake: “The label says 1 tsp, so I’ll use my coffee spoon.” Solution: Demand mL. Write it down. Say it out loud: “Five milliliters.”
- Mistake: “I gave it with food to hide the taste.” Solution: Mixing medicine with food can change how it’s absorbed. Only do this if the pharmacist says it’s safe.
- Mistake: “I didn’t know the syringe had to be cleaned.” Solution: Rinse the syringe with water after each use. Don’t reuse it for different medicines unless it’s thoroughly cleaned.

When Things Go Wrong
If you think you gave the wrong dose:- Don’t panic. Most small errors don’t cause harm.
- Call your pharmacist or doctor. They can tell you if the dose is dangerous.
- Don’t give another dose. Wait for instructions.
- Keep the bottle and syringe. They’ll help the provider understand what happened.
The Bigger Picture
Wrong-dose errors aren’t just about carelessness. They’re about systems that haven’t caught up. The U.S. spends $8.3 billion a year treating errors from liquid medications. That’s money spent on hospital stays, ER visits, and long-term care. But it’s also lives lost. The Institute for Safe Medication Practices says 14% of these errors lead to permanent harm or death. The good news? We know how to fix this. Use syringes. Use mL. Train staff. Use smart technology. Standardize labels. Enforce rules. Hospitals like Kaiser Permanente cut their liquid medication errors by 92% by doing just that. They gave every family a syringe. They trained staff. They built checks into their EHRs. They didn’t wait for perfection. They just started. You can do the same at home. You don’t need a hospital budget. You just need to know what to ask for-and when to say no.Frequently Asked Questions
Can I use a kitchen spoon if I don’t have a syringe?
No. Kitchen spoons vary in size and are never accurate. A teaspoon can hold between 2.5 mL and 7 mL. That’s a massive range for a child’s dose. Always use an oral syringe. If you don’t have one, ask your pharmacy for one or buy one online. It’s cheaper than a trip to the ER.
Why do pharmacies still give dosing cups?
Some still do because it’s cheaper and easier. Dosing cups cost less than syringes and are easier to dispense in bulk. But they’re far less accurate. The American Academy of Pediatrics and the ASHP have both said syringes should be the standard. If you’re given a cup, ask for a syringe instead. You have the right to the safest tool.
Is it safe to mix liquid medicine with juice or food?
Sometimes, but not always. Some medicines lose effectiveness when mixed with certain foods. Others become harder to measure accurately. Always check with your pharmacist before mixing. If you do mix it, make sure the child drinks the entire amount-don’t leave any behind in the cup.
What should I do if the label says “teaspoon”?
Call the pharmacy immediately. Ask them to re-label the prescription in milliliters (mL). The FDA has discouraged teaspoon use since 2010. You’re not being difficult-you’re protecting your child. If they refuse, go to another pharmacy. Many now offer mL-only labeling as standard.
Are oral syringes reusable?
They can be, but only if cleaned properly. Rinse the syringe with clean water after each use. Don’t reuse it for different medicines unless you’ve washed it thoroughly. If the plunger becomes sticky or the markings fade, replace it. A new one costs less than $2.
What’s the best way to store liquid medicine and syringes?
Keep the medicine in its original bottle, out of reach of children. Store the syringe inside the bottle cap or in a small labeled bag taped to the bottle. Never leave syringes lying around-they can get dirty, lost, or used by mistake for other purposes. Always keep them together.


Shayne Smith 5.12.2025
Just got my kid’s antibiotics yesterday-pharmacy gave me a cup. I asked for a syringe. They acted like I was asking for a unicorn. I told them I’d come back with a syringe from CVS if they didn’t give me one. They handed it over. Seriously, why is this still a fight?
Ashish Vazirani 5.12.2025
Who even uses teaspoons anymore?? This is why India’s healthcare is a joke-no standards, no discipline, no accountability. We’re still using spoon measurements while the West has moved to smart syringes and AI dose-checkers. Pathetic.
Mansi Bansal 5.12.2025
It is imperative to underscore, with the utmost gravity, that the utilization of non-standardized, non-metric, and non-regulated utensils-such as kitchen spoons-for the administration of pharmaceutical agents constitutes an egregious, potentially lethal, breach of clinical safety protocol. The variance in volume capacity among domestic utensils is not merely an inconvenience-it is an existential threat to pediatric integrity.
Myles White 5.12.2025
I’ve been a nurse for 18 years and I can tell you this: the biggest problem isn’t parents using spoons-it’s pharmacies refusing to give out syringes unless you beg for them. I’ve seen moms cry because they were told, ‘We don’t stock them.’ And then they go home and use a soup spoon because their kid won’t take the medicine any other way. It’s not negligence-it’s systemic neglect. Hospitals get $85k to switch to ENFit? Why can’t pharmacies spend $200 on a box of 100 syringes? It’s cheaper than one ER visit. And we all know how much those cost. I’ve watched kids get admitted because a mom thought ‘a teaspoon’ meant the same as the one she uses for sugar. It doesn’t. And no, you can’t ‘eyeball it.’ You really, really can’t.
Kumar Shubhranshu 5.12.2025
Syringes. mL. No spoons. Done.
Arjun Deva 5.12.2025
Wait… so you’re telling me the government knows this is happening but still lets pharmacies give out cups? And the FDA only ‘discouraged’ teaspoons in 2010? That’s not negligence-it’s a cover-up. Big Pharma doesn’t want you using syringes because they make more money off you buying new bottles when you mess up the dose. And don’t even get me started on how they’re pushing ‘dose packs’-that’s just another way to lock you into their system. This is all a scam. You’re being manipulated.
Nigel ntini 5.12.2025
Love this. Seriously. I’m a dad of two, and I used to think ‘a teaspoon’ was fine-until my daughter had a reaction from a mis-measured dose. Now I keep five syringes in the fridge with the meds. I label them with tape: ‘Amoxicillin - 5mL - Tue’. Simple. Safe. No guesswork. If your pharmacy doesn’t give you one, just say ‘I’m not leaving without it.’ You’re not being rude-you’re being responsible.
Saketh Sai Rachapudi 5.12.2025
Why are we letting foreigners tell us how to give medicine? In India, we’ve been using spoons for generations. Who are they to say it’s wrong? My cousin’s kid took medicine with a spoon for 3 years-no problems. This is just Western overthinking. We don’t need your syringes. We have common sense.
Jackie Petersen 5.12.2025
Okay but… what if the syringe breaks? Or gets lost? Or your kid bites it? Or you’re in a car and need to give it fast? Cups are faster. Easier. And honestly? Most people don’t even know what 5mL looks like. You’re telling me to trust a tiny plastic tube over a cup I’ve used for soup for 20 years? No thanks. This is fear-mongering disguised as ‘safety’.
Kenny Pakade 5.12.2025
So the solution is to make everyone buy a $2 syringe? What about poor people? What about people without cars to drive to CVS? This is a luxury solution for rich folks who care more about ‘accuracy’ than real life. Meanwhile, the real problem is that meds are too damn expensive and no one checks if the dose even makes sense. But sure, blame the spoon.
Clare Fox 5.12.2025
It’s funny how we treat medicine like it’s a math problem. ‘Measure 5mL exactly.’ But what if the kid spits half? What if the medicine settles at the bottom? What if the syringe’s plunger sticks? We act like precision is the only thing that matters… but life isn’t a lab. Maybe we need to stop obsessing over 0.1mL differences and start asking why we’re giving these drugs in the first place. Why is a 2.5mL dose even necessary? Is there a gentler way? Maybe the real issue isn’t the spoon-it’s that we’re medicating everything, and we’ve forgotten how to listen to the body.