Malignant Hyperthermia Preparedness Assessment Tool
This tool helps assess whether a hospital is properly prepared to handle malignant hyperthermia emergencies based on key indicators.
MH Preparedness Assessment
The hospital appears well-prepared to handle malignant hyperthermia emergencies. This means they have the critical resources needed to initiate life-saving treatment quickly.
Key indicators: dantrolene on hand ($144,000 worth), MH emergency carts within 30 seconds of ORs, and staff trained through annual MH drills.
Imagine going in for a routine surgery-maybe a tonsillectomy or wisdom tooth removal-and waking up in a medical crisis. Your heart is racing, your body is overheating, and your muscles are locked tight. This isn’t a nightmare. It’s malignant hyperthermia, a rare but deadly reaction to certain anesthesia drugs. It can strike anyone, even if they’ve had anesthesia before with no issues. And if it’s not caught fast, it can kill.
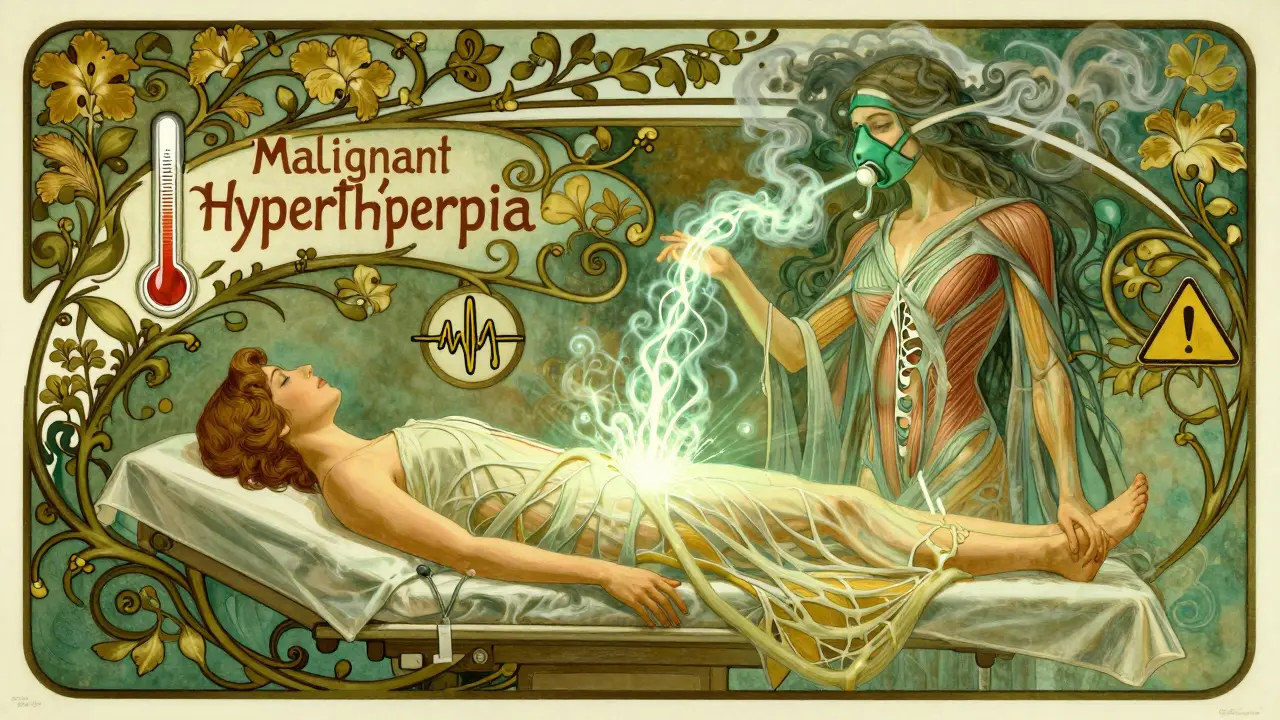
What Exactly Is Malignant Hyperthermia?
Malignant hyperthermia (MH) is a genetic disorder that causes a dangerous spike in body temperature and muscle rigidity when someone with the mutation is exposed to specific anesthetics. It’s not an allergy. It’s not an overdose. It’s a flaw in how muscle cells handle calcium. In people with MH, certain drugs trigger a runaway release of calcium inside muscle cells. This forces muscles to contract nonstop, burning through oxygen and producing massive amounts of heat-sometimes raising body temperature to 109°F (43°C) in under an hour. The main triggers are volatile anesthetic gases like sevoflurane, desflurane, and isoflurane, and the muscle relaxant succinylcholine. These are common in general anesthesia. You might not even know you’re at risk until it happens. About 70% of cases are linked to mutations in the RYR1 gene, which controls calcium release in muscles. Another 1% are tied to CACNA1S. The rest? Still being studied.How Do You Know It’s Happening?
The signs don’t wait for the surgery to end. They start fast-often within minutes of the anesthetic being given. Early warning signs include:- Unexplained fast heart rate (over 120 beats per minute)
- Rising carbon dioxide levels in exhaled breath (end-tidal CO2 above 55 mmHg)
- Unusual muscle stiffness, especially in the jaw (masseter muscle rigidity)
- Rapid breathing
- Body temperature climbing above 104°F (40°C)
Why Do Some People Get It and Others Don’t?
MH runs in families, but not always. About 29% of cases happen in people with no known family history. That’s why you can’t rely on asking your relatives. Even if no one in your family has had it, you could still carry the gene. The mutation is inherited in an autosomal dominant pattern-meaning you only need one copy from either parent to be at risk. Children are more vulnerable. MH occurs about 1 in 3,000 pediatric surgeries, especially during tonsillectomies. That’s why anesthesiologists watch kids extra closely. But adults aren’t safe either. Most cases happen in otherwise healthy people with no prior medical problems. That’s the scariest part-it doesn’t discriminate.
The Lifesaving Treatment: Dantrolene
There’s one drug that stops malignant hyperthermia in its tracks: dantrolene. It works by blocking calcium release in muscle cells, calming the runaway contraction. But it’s not easy to use. The old version, Dantrium®, took 22 minutes to mix and get ready. In a crisis, that’s too long. The newer version, Ryanodex®, dissolves in just one minute. It’s now the gold standard. Each vial costs about $4,000. Hospitals must keep at least 36 vials on hand-$144,000 worth of emergency medication-just in case. That’s a huge burden, especially for small or rural hospitals. Treatment isn’t just about the drug. You also need to:- Stop all triggering anesthetics immediately
- Give 100% oxygen at 10 liters per minute
- Hyperventilate to flush out excess CO2
- Cool the patient with ice packs, cold IV fluids, or even bypass machines
- Treat high potassium with insulin and glucose
- Protect the kidneys with mannitol and furosemide
How Hospitals Are Getting Better at Handling MH
In the 1970s, MH killed 80% of those who had it. Today, thanks to dantrolene and better protocols, that number is down to 5%. That’s progress. But it’s not perfect. The Malignant Hyperthermia Association of the United States (MHAUS) runs a 24/7 hotline (1-800-644-9737) that connects anesthesiologists with experts during emergencies. Since 1997, it’s helped cut mortality by 37%. Many top hospitals now have “MH carts”-pre-stocked emergency kits with dantrolene, syringes, cooling gear, and blood gas tools-within 30 seconds of every operating room. Mayo Clinic cut their treatment time from 22 minutes to under 5 minutes after implementing this system. The American Society of Anesthesiologists now requires annual MH simulation drills for all anesthesia teams. Residents need at least three practice scenarios before they can reliably spot early signs. Still, 42% of MH cases happen in places that skip basic preoperative screening. That’s unacceptable.
What You Can Do as a Patient
You can’t prevent MH on your own-but you can reduce your risk. If you’ve had a bad reaction to anesthesia before, or if someone in your family died suddenly during surgery, tell your anesthesiologist. Ask if they have dantrolene on hand. Ask if they’ve trained for MH emergencies. Genetic testing for RYR1 mutations is available. It costs between $1,200 and $2,500 and is about 95% accurate for known mutations. If you test positive, you’ll need to wear a medical alert bracelet and ensure any future surgeries use non-triggering anesthetics like propofol or ketamine. And if you’re scheduled for surgery, ask: “Do you have a plan if malignant hyperthermia happens?” If they hesitate or don’t know, consider transferring to a facility with better protocols.What’s Coming Next?
The future of MH care is getting faster and smarter. In 2024, the FDA is expected to approve an intranasal version of dantrolene for use before reaching the hospital-huge for ambulances and rural clinics. Researchers are testing new drugs like S107 that stabilize the RYR1 channel directly. And by 2027, early CRISPR trials may aim to fix the mutation at the DNA level. Meanwhile, anesthesia machines are getting smarter. Epic Systems’ 2024 software update now flags MH in real time-when three signs (high CO2, fast heart rate, rising temperature) appear together, it triggers an automatic alert. This could catch cases even before the anesthesiologist notices.Final Thoughts
Malignant hyperthermia is rare, but it doesn’t care how healthy you are, how young you are, or how routine your surgery seems. It’s silent until it strikes. But now, we know how to stop it. We have the drugs. We have the protocols. We have the training. The problem isn’t science. It’s access. It’s awareness. It’s whether the hospital down the road has the $144,000 in dantrolene on the shelf-or if they’re still hoping they won’t need it. If you’re facing surgery, don’t assume it’s safe. Ask the questions. Demand the prep. Because in a moment, a single drug can turn a routine procedure into a battle for life.Can malignant hyperthermia happen during local anesthesia?
No. Malignant hyperthermia is triggered only by specific general anesthetics-volatile gases like sevoflurane or the muscle relaxant succinylcholine. Local anesthetics like lidocaine or bupivacaine do not trigger MH. If you’re only getting a numbing shot or regional block (like an epidural), your risk is effectively zero.
If I had surgery before without problems, am I safe?
Not necessarily. MH can occur on the first exposure to triggering agents. About 29% of cases happen in people with no prior history or family background. Just because you’ve had anesthesia before doesn’t mean you’re immune. The gene mutation is there from birth-it just needs the right trigger to activate.
Is there a blood test to check for malignant hyperthermia?
There’s no routine blood test. The most reliable diagnostic method is the caffeine-halothane contracture test (CHCT), which requires a muscle biopsy. But this is only done at specialized centers and usually for people with strong family history or previous reaction. Genetic testing for RYR1 and CACNA1S mutations is more common now and can identify about 70-80% of known cases, though it can’t catch every possible mutation.
Can I get genetic testing for MH before surgery?
Yes. Genetic testing for RYR1 and CACNA1S mutations is available through over 27 certified labs in the U.S. It’s recommended if you or a close relative had a suspected MH episode, unexplained death during anesthesia, or unexplained muscle problems. The test costs $1,200-$2,500 and takes a few weeks. If positive, you’ll avoid triggering anesthetics for life.
What happens if a hospital doesn’t have dantrolene?
This is a life-threatening situation. Without dantrolene, the mortality rate jumps to over 70%. In such cases, the team must immediately stop triggering agents, hyperventilate, cool the patient, and transfer them to a facility with dantrolene. Emergency services should be called. The MHAUS hotline (1-800-644-9737) can help locate the nearest stocked facility. The FDA now requires all facilities performing general anesthesia to have an MH emergency kit-so lack of dantrolene is a serious violation of safety standards.
Is malignant hyperthermia the same as heat stroke?
No. While both involve high body temperature, heat stroke is caused by environmental overheating and dehydration. MH is a genetic, drug-induced muscle disorder. The body temperature spike in MH is caused by uncontrolled muscle contractions, not external heat. Treatment is completely different: cooling helps in both, but only dantrolene stops MH at its source.
Can I still have surgery if I have a positive MH gene test?
Yes, absolutely. People with confirmed MH mutations can have safe surgeries using non-triggering anesthetics like propofol, ketamine, lidocaine, or regional anesthesia. The key is planning. You must inform your surgical team in advance and ensure they avoid all volatile gases and succinylcholine. With proper precautions, your risk is near zero.

Dana Termini 5.01.2026
Malignant hyperthermia is one of those silent killers that no one talks about until it’s too late. I had a cousin who almost died during a wisdom tooth extraction-no family history, no warning. They didn’t even have dantrolene on hand at that little outpatient clinic. It took 45 minutes to transfer her to a real hospital. She’s fine now, but I’ll never forget how fast it all went south.
Wesley Pereira 5.01.2026
So let me get this straight-we’re spending $144K on a drug that might never be used… but if it IS used, we’re screwed without it? Classic healthcare logic. Meanwhile, my local hospital still uses the 1990s version of Dantrium because ‘budget constraints.’ Funny how ‘life-saving’ only means something when the insurance company says it’s worth the cost. #CapitalismInMedicine
Isaac Jules 5.01.2026
Anyone else find it hilarious that people think ‘I’ve had anesthesia before so I’m safe’? That’s like saying ‘I’ve driven a car before so I can’t die in a crash.’ You’re not immune-you’re just lucky so far. And if your anesthesiologist doesn’t know what MH is, you’re not getting surgery there. Period. Stop being passive. Ask. Demand. Or don’t complain when your kid turns into a human furnace.
Amy Le 5.01.2026
🚨🇺🇸 AMERICA STILL HAS HOSPITALS WITHOUT DANTRYLENE?!?!? 🚨 We have Mars rovers but can't afford $144K for a drug that saves lives?? This is why I hate this country. We spend billions on weapons but can't stock a vial that stops a kid from cooking alive. 🤬 Also, CRISPR for MH by 2027? Please. It'll be 2035 before the FDA approves it. We're a nation of outrage, not action.
Pavan Vora 5.01.2026
Dear friends, I am from India, and here in our small city hospital, we do not have dantrolene at all. We use only local anesthesia for dental surgeries, because we are afraid. My brother had a surgery, and they used sevoflurane, and he had a fever after, but no one knew why. Now, I tell everyone: avoid general anesthesia if you can. Please, be careful. Thank you for this article.
Stuart Shield 5.01.2026
It’s wild how something so terrifyingly specific-like a single gene glitch triggered by a gas you breathe-can be the difference between walking out of the OR and never waking up. We’ve got AI predicting cancer, robots stitching wounds, but we still rely on a single, expensive, temperamental drug to stop a biological firestorm. It’s not just medicine-it’s a high-stakes game of Russian roulette with your DNA. And yet, we treat it like a footnote in a consent form.
Lily Lilyy 5.01.2026
You can do this! Always ask questions before surgery. Your life matters. If you're nervous, bring a friend to help you ask. Hospitals want you to be safe. Don't be shy-your courage today could save your life tomorrow. 💪❤️
Susan Arlene 5.01.2026
so like… if you’ve never had anesthesia before, you’re basically playing russian roulette with your body? cool. guess i’ll just not get surgery then. 🤷♀️
Joann Absi 5.01.2026
They say it’s rare… but what if it’s YOU? What if it’s your child? Your spouse? Your best friend? You think it won’t happen because it’s ‘rare’? That’s the same thinking that got people to ignore the warning signs before 9/11. We don’t need statistics-we need action. We need to treat every patient like they’re one wrong breath away from dying. And if your hospital doesn’t have dantrolene? That’s not negligence-that’s murder by bureaucracy.
Ashley S 5.01.2026
Why are we even using these dangerous gases in the first place? We have propofol. We have ketamine. We have spinal blocks. Why are we risking lives for ‘convenience’? It’s not about cost-it’s about laziness. Anesthesiologists don’t want to learn new protocols. Hospitals don’t want to spend the money. Patients don’t know to ask. It’s a perfect storm of apathy. And now people are dying. Again.
Tom Swinton 5.01.2026
I work in a rural ER, and I’ve seen this firsthand. A 19-year-old girl came in after a tonsillectomy-her temp was 107.8, her CK was through the roof, her urine was black. We had one vial of dantrolene. We gave it. We cooled her with ice baths, IV fluids, fans, everything. We called MHAUS. They talked us through it for 90 minutes. She survived. But the next day, the hospital administrator told us we couldn’t afford to keep more than two vials. Two. For a town of 80,000. I cried in the supply closet. This isn’t a medical issue. It’s a moral failure. And we’re all complicit.
Gabrielle Panchev 5.01.2026
Actually, the real issue isn’t dantrolene-it’s that we still don’t screen for MH before surgery. Why aren’t we doing genetic testing as standard for all patients under 30? It’s cheaper than a single CT scan. And if you’re going to spend $144,000 on stockpiling drugs, why not spend $10,000 on universal screening? We screen for Down syndrome before birth, but we won’t screen for a condition that kills healthy young people in minutes? That’s not healthcare. That’s gambling with human lives-and the house always wins.